CALIFORNIA - CORONARY CTA PRIOR-AUTHORIZATION INFORMATIONAL GUIDE
Updated April 5th, 2017
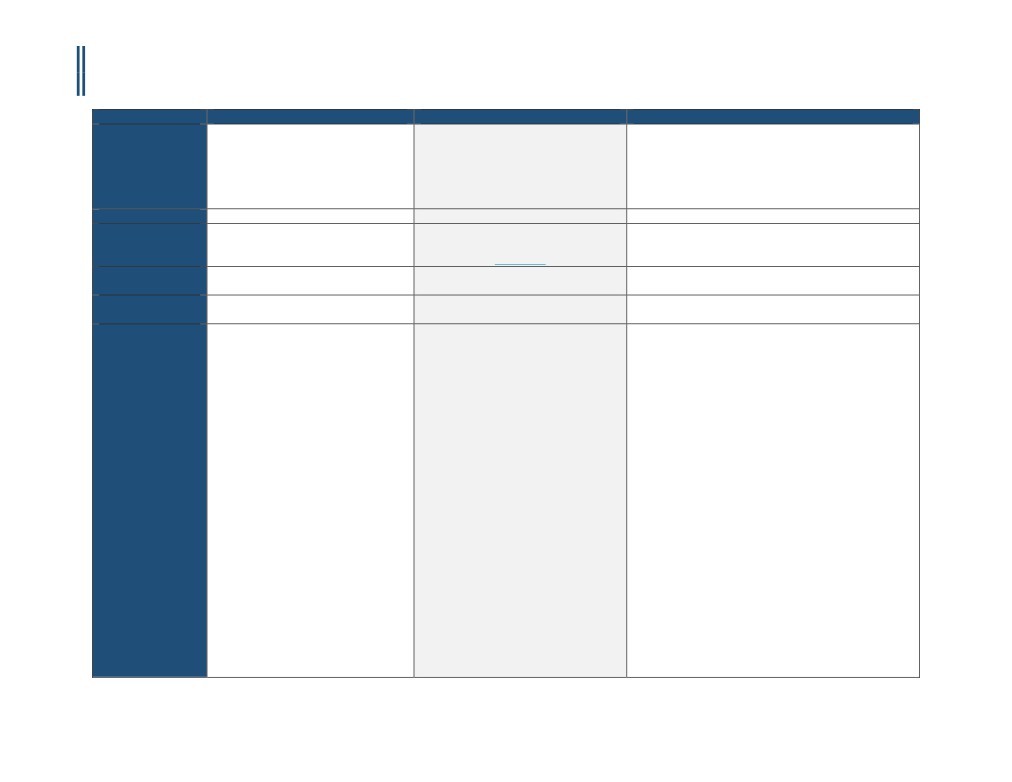
Payer
Anthem BlueCross BlueShield
Blue Shield of California
Health Net
Policy Name
Coronary Artery Imaging: Contrast-
Contrast-Enhanced Coronary Computed
eviCore Cardiac Imaging Guidelines
Enhanced Coronary Computed
Tomography Angiography for Coronary
Tomography Angiography (CCTA),
Artery Evaluation
Coronary Magnetic Resonance
Angiography (MRA), and Cardiac
Magnetic Resonance Imaging (MRI)
Policy #
RAD.00035
Section: 6.0 Radiology
CD-8~CT HEART and CCTA
RBM
AIM Specialty Health® (AIM)
National Imaging Associates
eviCore (Product line and POS dependent)
Applicable CPT
75574
75574
75574
Code(s)
Applicable ICD
Not Listed
Not Listed
Not Listed
Code(s)
Covered
Contrast-enhanced coronary computed
• Contrast-enhanced coronary computed
• For symptomatic individuals who have a very low, low, or
tomography angiography (CCTA) is
tomography angiography (CCTA) may be
intermediate pretest probability of CAD, CCTA may be
considered medically necessary for the
considered medically necessary for
used in the following situations:
evaluation of suspected anomalous
evaluation of patients without known
o Unable to perform either an exercise or
coronary arteries:
coronary artery disease and acute chest
pharmacologic imaging stress test
• For the evaluation of suspected
pain in the emergency department
o Stress test (treadmill or imaging stress test) is
anomalous coronary arteries:
setting.
uninterpretable, equivocal, or a false positive is
o In pediatric individuals (age < 18
• Contrast-enhanced coronary computed
suspected
years) either before or after
tomography angiography (CCTA) may be
o Replace performance of invasive coronary angiogram
conventional angiography; or
considered medically necessary for
• For symptomatic individuals, evaluate post-CABG graft
o In adults (age 18 and over) when
evaluation of patients with stable chest
patency when only graft patency is a concern and
conventional angiography has
pain and meeting guideline criteria for a
imaging of the native coronary artery anatomy is not
been unsuccessful or has provided
noninvasive test in the outpatient
needed, such as in early graft failure
equivocal results and the results
setting (see Policy Guidelines).
• For symptomatic individuals with unsuccessful
could impact treatment.
• Contrast-enhanced coronary computed
conventional coronary angiography
tomography angiography (CCTA) may be
• Additional Indications:
considered medically necessary for
o Re-do CABG: To identify whether bypass grafts are
evaluation of anomalous (native)
located directly beneath the sternum, so that
coronary arteries in patients in whom
alternative ways to enter the chest can be planned
they are suspected.
o Evaluate coronary artery anomalies and other
complex congenital heart disease of cardiac
Policy Guidelines
chambers or great vessels
The 2012 collaborative medical
o Anomalous coronary artery(ies) suspected for
association guidelines for the diagnosis
diagnosis or to plan treatment and less than age 40
and management of patients with stable
1
CCM-100-100-B
CALIFORNIA - CORONARY CTA PRIOR-AUTHORIZATION INFORMATIONAL GUIDE
Updated April 5th, 2017
heart disease (Fihn et al, 2012) list several
with a history that includes one or more of the
class I recommendations on use of
following
noninvasive testing in patients with
▪ Persistent exertional chest pain and normal stress
suspected stable ischemic heart disease. A
test
class I recommendation indicates that a
▪ Full sibling(s) with history of sudden death
test should be performed. In general,
syndrome before age 30 or with documented
patients with at least intermediate risk
anomalous coronary artery
(10%-90% risk by standard risk prediction
▪ Resuscitated sudden death and contraindications
instruments) are recommended to have
for conventional coronary angiography
some type of test, the choice depending
o Unexplained new onset of heart failure
on interpretability of the
o Evaluation of newly diagnosed congestive heart
electrocardiogram, capacity to exercise,
failure or cardiomyopathy
and presence of comorbidity.
▪ No prior history of coronary artery disease, the
ejection fraction is less than 50 percent, and low
or intermediate risk on the pre-test probability
assessment AND
▪ No exclusions to cardiac CT angiography
▪ No cardiac catheterization, SPECT, cardiac PET, or
stress echocardiogram has been performed since
the diagnosis of congestive heart failure or
cardiomyopathy
o Ventricular tachycardia (6 beat runs or greater) if
CCTA will replace conventional invasive coronary
angiography
o Equivocal coronary artery anatomy on conventional
cardiac catheterization
o Newly diagnosed dilated cardiomyopathy
o Preoperative assessment of the coronary arteries in
patients who are going to undergo surgery for aortic
dissection, aortic aneurysm, or valvular surgery if
CCTA will replace conventional invasive coronary
angiography”
o Vasculitis/Takayasu’s/Kawasaki’s disease
o Cardiac Trauma: Chest CTA (CPT®71275) and CCTA
(CPT®75574) are useful in detecting aortic and
coronary injury and can help in the evaluation of
myocardial and pericardial injury
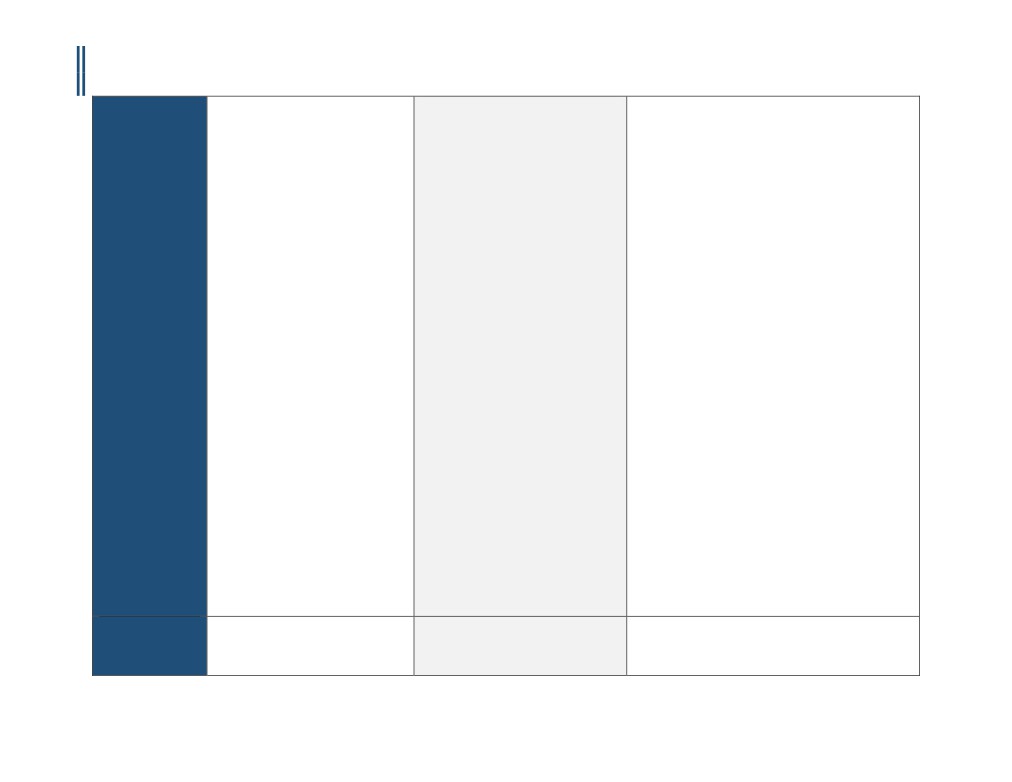
Not Covered /
• Coronary computed tomography
• Contrast-enhanced coronary computed
• Irregular heart rhythms
Investigational and
angiography (CCTA) is considered
tomography angiography (CCTA) is
• Multifocal Atrial Tachycardia (MAT)
Not Medically
investigational and not medically
considered investigational for all other
• Inability to lie flat
Necessary
necessary for all other indications,
indications.
• Body mass index of 40 or more
2
CCM-100-100-B
CALIFORNIA - CORONARY CTA PRIOR-AUTHORIZATION INFORMATIONAL GUIDE
Updated April 5th, 2017
including, but not limited to, the
• Inability to obtain a heart rate less than 65 beats per
following:
minute after beta-blockers
o Screening for coronary artery
• Inability to hold breath for at least 8 seconds
disease (CAD), either in
• Renal Insufficiency
asymptomatic individuals or as
• Asymptomatic patients and routine use in the evaluation
part of a preoperative evaluation;
of the coronary arteries following heart transplantation
or
• CCTA should not be performed if there is extensive
o Diagnosis of CAD, in individuals
coronary calcification (calcium score >1000)
with acute or non-acute
• Evaluation of coronary stent patency (metal artifact
symptoms, or after a coronary
limits accuracy)
intervention; or
• Evaluation of left ventricular function following
o As a technique to evaluate cardiac
myocardial infarction or in chronic heart failure
function
• Evaluation of patients with postoperative native or
prosthetic cardiac valves who have technically limited
echocardiograms, MRI or TEE. Patients with
indeterminate echocardiogram should undergo MUGA
(CPT®78472 or CPT®78494) or cardiac MRI
• First test in evaluating symptomatic patients (e.g. chest
pain)
• Irregular heart rhythms
• High pre-test probability for CAD—rather, these patients
should undergo conventional coronary angiography,
especially if an interventional procedure (e.g., PCI) is
anticipated
• Identification of plaque composition and morphology
• Myocardial perfusion and viability studies
• Preoperative assessment for non-cardiac, nonvascular
surgery
• Repeat or routine follow-up of CAD with CCTA
• There is insufficient evidence to support routine use of
Coronary Computed Tomography Angiography (CCTA) in
the evaluation of the coronary arteries following heart
transplantation.
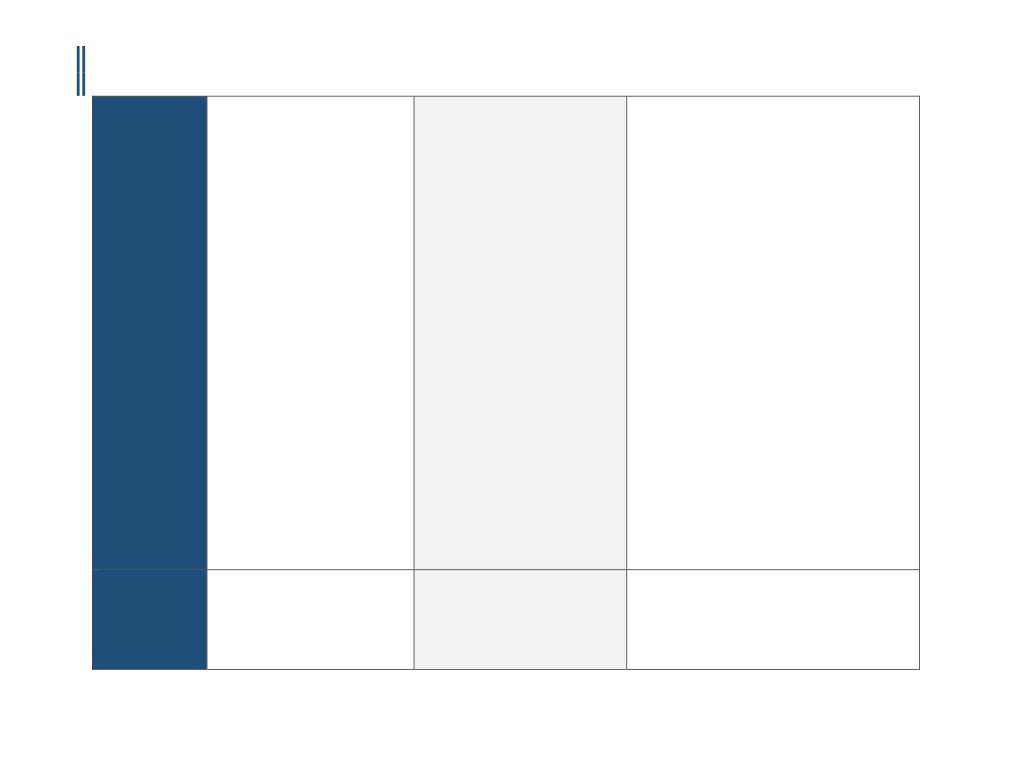
Payer Specific
• Please provide the following
Requirements
documentation (if/when requested):
o History and physical and/or
consultation notes including:
▪ Current symptoms and clinical
findings
▪ Reason for the procedure
3
CCM-100-100-B
CALIFORNIA - CORONARY CTA PRIOR-AUTHORIZATION INFORMATIONAL GUIDE
Updated April 5th, 2017
o Diagnostic radiology reports
pertaining to request (e.g.,
echocardiogram, transesophageal
echocardiogram, MRI)
o Post Service
▪ Radiology procedure report(s)
• Within five days before the actual date
of service, the provider must confirm
with Blue Shield that the member's
health plan coverage is still in effect.
Blue Shield reserves the right to revoke
an authorization prior to services being
rendered based on cancellation of the
member's eligibility. Final
determination of benefits will be made
after review of the claim for limitations
or exclusions.
• Questions regarding the applicability of
this policy should also be directed to
the Prior Authorization Department.
Please call 1-800-541-6652 or visit the
Provider Portal
Effective Date
04/05/2016
2/1/2017
3/18/2016
Last Review/
02/04/2016
4/3/2009
12/31/2015
Original Policy Date
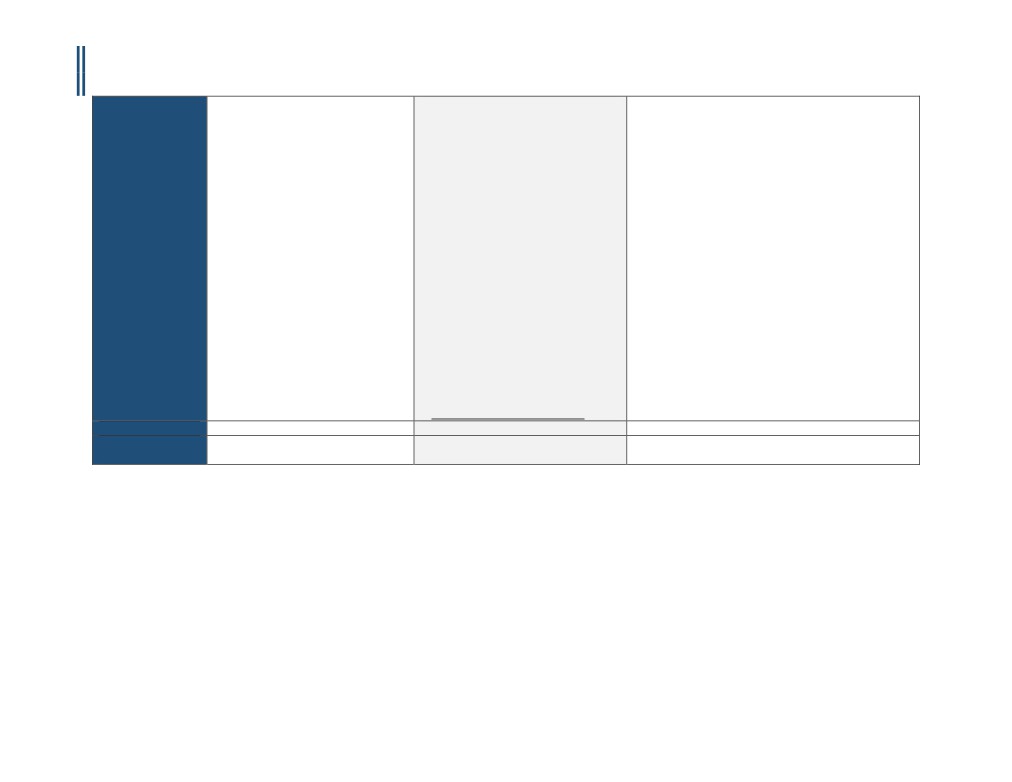
SUGGESTED DOCUMENTATION TO NAVIGATE PRE-AUTHORIZATION
For instances when the indication is medically necessary, clinical evidence is required to determine medical necessity. For instances when the indication is investigational, you
may submit additional information to the Prior Authorization Department. The following documentation is recommended in order to ensure that pre-authorization can be
secured in a timely and efficient manner:
1.
Medical chart notes - all notes from the patient chart related to the requested procedure, including patient’s current cardiac status/ symptoms, cardiac
factors, and indications.
2.
Relevant patient information, including:
▪ Patient age, height, weight, and BMI
▪ Family history of heart problems (including relationship to member, age at diagnosis, type of event, etc.)
▪ Medical history (e.g. diabetes, hypertension, stroke arrhythmia, etc.)
▪ Cardiac risk factors
▪ Previous cardiac treatments, surgeries, or interventions
▪ Problems with exercise capacity
4
CCM-100-100-B

CALIFORNIA - CORONARY CTA PRIOR-AUTHORIZATION INFORMATIONAL GUIDE
Updated April 5th, 2017
▪ Ordering provider information
▪ Imaging provider information
▪ Imaging exam(s) being requested (body part, right, left, or bilateral)
▪ Patient diagnosis (suspected or confirmed)
3.
Diagnostic or imaging reports from previous tests (exercise stress test, echocardiography, stress echocardiography, MPI, coronary angiography, etc.)
4.
Symptom history (onset, course, new or changing symptoms) related to all pertinent cardiac conditions, such as heart muscle/ valvular disease, structural
abnormality, infection, exposure to toxins/ chemotherapy, etc.
5.
Examination results, including evaluation of hypertension, heart failure, cardiomyopathy, abnormal rhythm, pulmonary embolus, congenital condition, etc.
6.
Any other documentation that supports the need for the procedure
DISCLAIMER: The information provided in this document is general information only and is not provided as legal advice, nor is it advice about how to code, complete, or submit any particular claim for
payment for health care services or goods. This information provides only an overview of HeartFlow’s understanding of current coverage policies for a select number of payers, and may not provide
all the information necessary to understand a particular patient’s benefits or payer’s coverage policies and prior authorization requirements. The information provided may not be comprehensive or
complete. It is the responsibility of the health care provider, such as a hospital or a physician to verify coverage and prior authorization requirements, submit complete, accurate and appropriate bills
or claims for payment that comply with applicable laws and regulations and third-party payer requirements, and to determine the appropriate codes, charges, and modifiers that the provider uses for
those purposes. Third-party payers may have policies and coding requirements that differ from those described here, and such policies can change over time.
HeartFlow disclaims any responsibility for claims submitted by health care physicians or others. Physicians should check and verify current policies and requirements with the payer for each patient.
HeartFlow endorses the best practice that all coding and billing submissions to payers be truthful and not misleading, and that providers make full disclosures to the payer about how the service has
been used. HeartFlow cannot guarantee success in obtaining payment for products and services.
Current Procedural Terminology (CPT) copyright 2016.
All rights reserved. CPT® is a registered trademark of the American Medical Association (AMA). Fee schedules, relative value units, conversion factors and/or related components are not assigned by
the AMA, are not part of CPT coding, and the AMA is not recommending their use.
The International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10) is maintained by the National Center for Health Statistics and the Centers for Medicare and Medicaid
Services.
References:
1.
“Cardiac Checklist (Health Plan).” RadMD, http://www1.radmd.com/media/459739/template-cardiac-checklist-magellan-hc-logo-4-1-2016.pdf. Accessed 25 October 2016.
2.
“AIM Specialty Health (AIM) Ordering Physician/Provider Quick Tips for Diagnostic Imaging Management Programs.” Anthem,
https://www11.anthem.com/provider/nh/f5/s2/t0/pw_ad087257.pdf. Accessed 25 October 2016.
5
CCM-100-100-B