
Standards of practice of computed
tomography coronary angiography
(CTCA) in adult patients
Standards of practice of computed tomography
2
coronary angiography (CTCA) in adult patients
Contents
Foreword
3
References
16
1. Recommended standards
4
Appendix 1. Contributing authors and
18
reviewers
2. Introduction
5
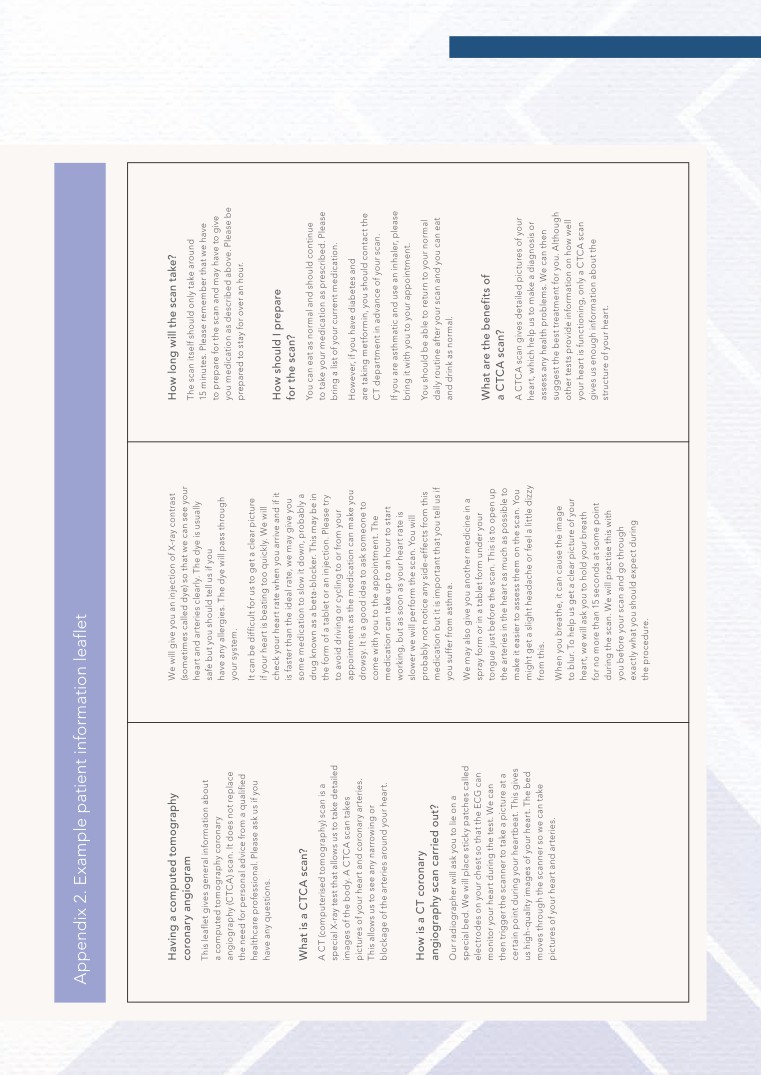
Appendix 2. Example patient information
19
3. Patient information prior to CTCA
6
leaflet
4. Important patient-specific information
6
Appendix 3. CTCA patient safety
21
before the scan
questionnaire
5. Safe drug administration in preparation
7
Appendix 4. Pharmacokinetics of
22
for CTCA
beta-blockers used for heart rate reduction
prior to CTCA
6. Iodine-based contrast safety
8
Appendix 5. Treatment of adverse events
23
7. CT scanner technical requirements
9
after heart rate-lowering medication
8. Scanning modes
10
Appendix 6. Monitoring checklist for
24
adult patients receiving beta-blockers
9. Image quality and radiation dose
12
for lowering heart rate +/- sublingual
optimisation
GTN for CTCA
10. The use of iodinated contrast medium
13
Appendix 7. Auditing patient radiation
25
in CTCA
doses in CTCA
11. Patient care during and after the scan
15

Standards of practice of computed tomography
3
coronary angiography (CTCA) in adult patients
Foreword
Together with the Royal College of Physicians (RCP) and the
British Society of Cardiovascular Imaging (BSCI), The Royal College of
Radiologists (RCR) has produced this document, which brings together
the latest guidance on departmental standards of practice required to
deliver safe computed tomography coronary angiography (CTCA)
to adult patients.
Appropriate training of all healthcare professionals involved in delivering
CTCA to adult patients with known or suspected coronary artery
disease is essential, together with the most appropriate and up-to-date
CT scanners with the ability to modulate dose.
We would like to take this opportunity to thank those who have
worked together to produce this document, with special thanks to
Dr Stephen Harden, who chaired the document development working
party (for a full list of working party members and contributors please
see Appendix 1).
The RCR has committed to reviewing all relevant publications in line with
the recommendations of the Francis report and, where appropriate,
applying the category of standard defined by Francis (fundamental,
enhanced or developmental).1 This document contains standards that
fall within the enhanced category.
Dr Pete Cavanagh
Vice-President, Faculty of Clinical Radiology
The Royal College of Radiologists
Dr Andrew Goddard
Registrar
The Royal College of Physicians
Dr Stephen Harden
President
The British Society of Cardiovascular Imaging

Standards of practice of computed tomography
4
coronary angiography (CTCA) in adult patients
Standard 6
1. Recommended
standards
Prospective ECG gating should be
the firstline default technique, used
Standard 1
whenever possible and practical.
Staff should be trained in
Retrospective ECG gating should
cardiovascular CT according
only be used in specifically selected
to national/international guidelines,
cases (page 10).
undertake continuing professional
Standard 7
development (CPD) activities in
CTCA and cardiovascular CT and
The radiation dose administered
should be trained in basic life
should be as low as possible,
support techniques (page 5)
commensurate with diagnostic
(for CTCA training guidelines see
image quality. Radiation doses and
image quality should be routinely
and regularly audited and
Standard 2
benchmarked against other national
All patients should receive a letter/
centres (Appendix 7).
information leaflet giving an outline
Standard 8
of the procedure, the preparation
required and local site details
The iodinated contrast medium
(Appendix 2).
delivery protocol should be
adjusted for each patient group and
Standard 3
according to the scanner being
All patients should have a risk
used (page 13).
assessment by a member of staff to
Standard 9
ensure that it is safe for them to
undergo the scan (Appendix 3).
The patient should be reviewed by
an appropriately qualified member
Standard 4
of staff prior to discharge from the
Provided it is safe and practical
scanning department (page 15).
to do so, heart rate-controlling
drugs should be administered
so that the patient’s heart rate is
<65 beats per minute during the
scan (Appendices 4-6).
Standard 5
The scanner used should be
specifically set up for CTCA and be
of 64 slices or greater, with cardiac
software and electrocardiogram
(ECG) gating (page 9).

Standards of practice of computed tomography
5
coronary angiography (CTCA) in adult patients
As a result of the frequent need to
These guidelines have been
2. Introduction
administer heart rate-controlling
created using a combination of
CTCA has become a well-
drugs, CTCA practitioners also
evidence-based practice and an
recognised imaging technique in
need to be aware of the potential
accepted consensus of expert
the investigation of patients with
complications and interactions of
opinion of best practice where this
chest pain. The indications for
these drugs and how they should
evidence does not exist. A list of
CTCA are also established and it is
be managed. All members of the
the contributors to this document is
part of nationally and internationally
CTCA team should have frequent
given in Appendix 1.
recognised imaging pathways. Its
and up-to-date training in basic life
clinical utility means that increasing
support, and at least one member
numbers of UK centres are
of the team should be trained in
establishing CTCA imaging
immediate life support.
Standard 1
programmes.
Resuscitation facilities should be
Staff should be trained in
Recommendations exist for CTCA
immediately available.
cardiovascular CT according
training, accreditation and
It is important for the CTCA
to national/international
revalidation requirements for
imaging team to establish close
guidelines, undertake
radiologists and cardiologists
links with referring clinical teams.
continuing professional
A clear understanding of how the
development (CPD) activities
and there are guidelines on how
scan is performed and the
in CTCA and cardiovascular
these should be reported.2-4 This
information it is capable of
CT and should be trained in
document focuses on departmental
providing will mean that
basic life support techniques
standards of practice for CTCA in
appropriate patients are referred
(for CTCA training guidelines
adult patients from the time of
for this investigation. For example,
acceptance of the referral to the
a statement on the referral letter or
time that the patient leaves the
request card to the effect
imaging department having had the
that there are no known
scan. The emphasis is on achieving
contraindications to the
a good procedural outcome, with
administration of beta-blockers,
diagnostic-quality images obtained
glyceryl trintrate (GTN) or
in an environment in which the
intravenous contrast medium is very
safety of the patient is paramount.
helpful to the imaging team,
This document is divided into
although does not obviate the need
sections of recommended best
for the safety checks this document
practice before the start of the
outlines. It is also important that the
scan, during the scan and once the
referring clinical team is aware that
scan has been completed.
this test involves ionising radiation.
Radiologists and cardiologists will
The referrer and the CTCA imaging
be used to administering
team must follow the trust’s ionising
intravenous contrast medium and
radiation medical exposure
the urgent management required
regulations (IRMER) procedures for
to treat the complications which
carrying out medical exposures
sometimes occur with its use.
with ionising radiation.5 A medical
member of the CTCA imaging team
will act as the IRMER practitioner
and will be responsible for
confirming that the investigation
and the associated radiation dose
can be justified.
Standards of practice of computed tomography
6
coronary angiography (CTCA) in adult patients
An example checklist to be
3. Patient information
4. Important patient-
completed with the patient prior
prior to CTCA
specific information
to the scan is given in Appendix 3.
before the scan
The patient should understand why
This checklist has been created
the CTCA is being performed,
through the amalgamation of
When the patient attends the
having discussed this with the
departmental checklists that
CT department, they should have
referring doctor before the
have been used by UK cardiac
their height and weight measured
procedure. However, it is important
CT departments over several years,
to enable the body mass index
that the CT department performing
and the contained list of questions
(BMI) to be calculated. The patient’s
the scan sends additional
and checks are regarded as
blood pressure and heart rate
information to the patient before
best practice.
should be recorded. There are
they attend. This may take the form
important details of the patient’s
of a patient information leaflet
past medical history, current health
which explains the details of the
and current medications that must
Standard 3
procedure to help reduce patient
be documented before the scan
anxiety. The patient should be
All patients should have a risk
is performed.
encouraged to bring a list of all of
assessment by a member of
The specific questions relating
their current medications with
staff to ensure that it is safe
to contrast administration are
them. An example patient
for them to undergo the scan
the same as those for other
information leaflet is provided in
(Appendix 3).
iodinated contrast medium-based
Appendix 2.
tests. These focus on history of
allergy, recent contrast
administration, use of metformin
Standard 2
and renal function.
All patients should receive
The questions relating to beta-
a letter/information leaflet
blockers focus on specific
giving an outline of the
contraindications. It is important to
procedure, the preparation
determine if the patient is asthmatic
required and local site details
as beta-blockers should be
(Appendix 2).
administered with caution in
asthmatic patients and not used in
patients with severe asthma.
Beta-blockers should not be
administered in patients taking
verapamil, in patients with severe
aortic stenosis, restrictive
physiology, second- or third-degree
heart block or a history of transient
loss of consciousness.
GTN is usually well tolerated,
although it should not be used
in patients taking sildenafil
(Viagra [Pfizer, USA]) or other
such phosphodiesterase inhibitors
due to the risk of profound
hypotension.

Standards of practice of computed tomography
7
coronary angiography (CTCA) in adult patients
Intravenous dosing in CTCA
Monitoring
5. Safe drug
administration in
Metoprolol can be administered
All patients should have their blood
intravenously with the patient on
pressure and pulse measured and
preparation for CTCA
the scanner table. This method is
recorded before and after the
Heart rate control
now firstline in many UK centres and
administration of beta-blockers.
Heart rate reduction to <65 beats
has the advantage of heart rate
This should be done every 15-30
per minute (bpm) to minimise the
control being achieved quickly.
minutes and the patient should be
likelihood of motion artefacts on
Although the beta-blocker
seated or laying where they can be
derived images should be achieved
administration protocol is a matter
seen and monitored by staff, ideally
in all patients in which it is safe and
of local choice, a typical dose
in a dedicated monitoring bay.
practical to do so. The development
regime is as follows:
Treatment of symptomatic
of high-specification CT scanners
• Starting dose of 5 mg
bradycardia/hypotension
(for example, dual-source, >64 slice
intravenously over one minute
Patients who suffer symptomatic
scanners) means the likelihood of
followed by a saline flush, with
bradycardia and/or hypotension
diagnostic image quality is higher
re-administration of the same
should be treated with atropine
than for 64-slice CT when heart rate
dose every 2-3 minutes until
and/or glucagon, as detailed in
control is not achieved, but image
the heart rate is <65 bpm
Appendix 5. Consideration should
quality is improved even on these
• The maximum recommended
be given to a printed copy of
high-specification CT scanners
intravenous (IV) dose of
Appendix 5 being clearly displayed
when the heart rate is <65 bpm.6
metoprolol quoted in the British
on the wall of the scan room. IV
Beta-blockers
National Formulary is 15 mg,
fluids may be used for patients with
although doses up to 30 mg have
symptomatic hypotension in the
Beta-blockers should be used as
been quoted in the literature.7,8
absence of bradycardia. Other
the firstline drugs for the lowering
Some UK centres titrate up to 50
therapies, including transcutaneous
heart rate before a CTCA. They can
mg without reported adverse
pacing, temporary IV cardiac pacing
also have the beneficial effect of
events, and although there are
and calcium gluconate (such as in
reducing ectopic activity and the
reports of higher doses being
the setting of calcium channel
heart rate variability. Beta-blockers
administered, the benefit of these
blocker overdose) should be
should not be administered to
high doses is questionable.9
administered by emergency,
patients already taking verapamil
cardiology or critical care
due to the risk of ventricular
Oral dosing in CTCA
personnel. These treatments and
standstill and cardiac arrest.
Metoprolol is the most commonly
staff members should be readily
Metoprolol is the most commonly
used and studied beta-blocker in
accessible whenever beta-blockers
used beta-blocker in this context.
this setting. In patients with a
are administered.
It can be administered intravenously
resting heart rate >65 bpm the
or orally.
following regimes are typical:
• 50-100 mg one hour prior to
CTCA; or
• 50 mg 12 hours previously
followed by a further 50 mg one
hour before the scan.
These oral doses are then followed
by titrated IV metoprolol if the heart
rate remains >65 bpm.10
More detailed pharmacokinetics
are provided in Appendix 4.
Standards of practice of computed tomography
8
coronary angiography (CTCA) in adult patients
Other non-beta-blocker drugs
Headache is the most common
6. Iodine-based contrast
for heart rate control
side-effect of GTN administration
safety
(~10%) and patients may feel
Calcium channel blockers
slightly light-headed. GTN should
The preparation for contrast
Calcium channel blockers, such as
be used with caution in patients
medium administration to the
diltiazem and verapamil, can be
with a systolic blood pressure
patient should be in accordance
used to lower heart rate, such as in
<90 mmHg or severe aortic
with the RCR guidance on
patients where beta-blockers are
stenosis. Concomitant use with
Standards for Intravascular Contrast
contraindicated, but these are
phosphodiesterase inhibitors,
Agent Administration to Adult
generally not recommended. These
such as sildenafil, is contraindicated
Patients, Second edition.13
drugs should only be administered
as it can result in significant
Specific recommendations
following discussion with, or under
hypotension (Appendix 3).
the supervision of, a cardiologist in
• When a patient has a relative
Record keeping of drug
those cardiac CT units that are
contraindication to the
administration
radiology-led.
administration of IV iodinated
It is crucial to keep an accurate
contrast medium, measures to
Ivabradine
record of the drugs administered
reduce the possibility of contrast
Ivabradine reduces the
in CTCA. An example of a drug
reactions or nephrotoxicity should
depolarisation of the sino-atrial
administration and observation
be followed.
node (SAN) which leads to a
checklist is provided in Appendix 6.
• Contrast should be used with
reduction in heart rate. There is
caution in patients with borderline
some evidence of its use in lowering
or compromised renal function.
heart rate in patients prior to CTCA,
but it should be prescribed only
Standard 4
• The physician must be familiar
following discussion with the
with the manifestations of
Provided it is safe and
cardiology team.11
potential adverse reactions to the
practical to do so, heart
contrast medium.
Coronary artery vasodilation
rate-controlling drugs should
with GTN
be administered so that the
• The physician should be familiar
patient’s heart rate is <65
with the treatment of, and be
The administration of 1-2 sublingual
beats per minute during the
available to treat, any adverse
GTN tablets or 1-2 puffs of
scan (Appendices 4-6).
reactions to IV contrast medium.
sublingual GTN spray (400-800
micrograms [mcg]) is recommended
• All of the cardiac CT team should
just prior to the scan.12 The time to
have had training, and
peak effect is around six minutes so
demonstrate current competence,
timing of its use is important.
in basic life support.
Although there may be some
secondary reflex tachycardia, this
does not seem to be a problem in
practice. It may, however, lead to
further beta-blocker administration.
Most centres use GTN routinely to
increase coronary artery diameter,
but there is no data to suggest this
increases the accuracy of CTCA.
Standards of practice of computed tomography
9
coronary angiography (CTCA) in adult patients
General considerations
• The detector width must be
7. CT scanner technical
0.625 mm or less.
Minimum requirements
requirements
• The department must comply
• The gantry rotation time should
CT technology for cardiac imaging
with the Ionising Radiation
be <350 milliseconds (ms).18
is evolving rapidly. Historically,
Regulations 1999 and the Ionising
scanners from all vendors have had
• The Z-axis (craniocaudal
Radiation (Medical Exposures)
similar capabilities but over recent
direction) coverage must be at
Regulations 2000, and subsequent
years manufacturers have
least 20 mm, and at least 30 mm
amendments.5,15
developed a range of solutions for
is recommended (unless a
advanced cardiac CT. The new-
dual-source scanner is used) to
• A maintenance, servicing and
generation CT scanners offer
ensure a realistic scan time (and
repair programme must be in
improvements intended to address
therefore breath-hold) and to
place for all scanners within a
the previous limitations of CT for
minimise misalignment artefact.19
department (required by UK law).
cardiac imaging, particularly with
• The Z-axis resolution must be at
• The working life of a cardiac
improvements in temporal and
least 8 line pairs per centimetre
CT scanner should be around
spatial resolution, image
(lp/cm) at 10% modulation transfer
seven years, in keeping with the
misregistration and artefact
function (MTF).
manufacturer’s recommendations
reduction. This has resulted in
for maintenance. This may be
recent National Institute for
• The temporal resolution must
shorter in centres with high
Health and Care Excellence (NICE)
be less than 175 ms for a
throughput.16
guidance demonstrating the
single sector.
utility of CTCA in patients in who
• A quality assurance programme
• The scan plane resolution
CT imaging has traditionally been
should be in place, supervised by
must be at least 12.5 lp/cm at
challenging, as long as one of
appropriately trained
10% MTF.
the newer generation scanners
radiographers and medical
with dedicated cardiac capability
physicists (required by UK law).
Recommended best practice
is used.14
• The Z-axis coverage should
Scanner capabilities
Choice of technology
be approximately 30-40 mm
Minimum requirements
or greater.
The choice of scanner technology
• ECG gating with prospective
will ultimately depend on a number
• New-generation technology
and retrospective gating
of factors. This is likely to reflect
should be available when imaging
capability is required.
current preferences or service
patients who are difficult to scan.14
agreements and the requirements
• Dose modulation with the
Where this is not available in
of the existing service. It should be
ECG phase should be available for
the department, it must be
recognised that in all but the very
retrospectively gated scanning
accessible to a service via a
highest volume centres, the CT
to reduce the radiation dose to
cardiac network or other local
scanner will be used for non-cardiac
the patient.
arrangement.
imaging for a considerable amount,
• Pre-scan contrast timing
if not the majority, of the time.
assessment, either by automated
or visual bolus tracking or with
Standard 5
assessment of a test bolus, must
The scanner used should
be possible.
be specifically set up for
Hardware specification
CTCA and be of 64 slices or
Minimum requirements
greater, with cardiac software
and ECG gating.
• A 64-detector row (or above)
scanner is required.17 The
non-diagnostic rate of scanners
with fewer detector rows is
10% greater than those with
64 detectors.

Standards of practice of computed tomography
10
coronary angiography (CTCA) in adult patients
Retrospectively gated image
Dual-source scanners are also
8. Scanning modes
acquisition occurs with the X-ray
capable of prospective, helical
ECG gating is essential for coronary
tube continuously on over a number
acquisition using both X-ray sources
artery imaging. To minimise vessel
of cardiac cycles. During the scan,
to allow a high pitch acquisition.24
motion, points of relative cardiac
the projection data are tagged with
A heart rate of <60 beats per
rest are selected for image
the point in the ECG cycle at which
minute is generally required to
acquisition, usually at mid-diastole,
they were acquired. The required
provide a sufficiently long period of
or end-systole for slightly higher
points of the R-wave to R-wave (R-R)
diastasis. The second X-ray source
or variable heart rates. Previously,
interval are retrospectively selected
has a smaller field of view than the
ECG gating has been either
on the patient’s ECG (Figure 1A,
first, but it is sufficiently large for
retrospective (helical) or
opposite) and the corresponding
cardiac imaging.25
prospective (axial) but the advent
projection data are used to
of wide-detector arrays and
reconstruct the images at these
dual-source scanners has blurred
points. This can be used as a
these traditional boundaries.
problem-solving tool, for example,
Standard 6
Prospectively gated image
in patients with very high heart
Prospective ECG gating
acquisition takes place only at the
rates. Retrospective ECG gating
should be the firstline default
required phase of the cardiac cycle,
should only be used in specifically
technique, used whenever
which is anticipated by the scanner,
selected cases. The pitch should
possible and practical.
based on the patient’s ECG (Figure
not be less than 0.2. Adaptive
Retrospective ECG gating
1C, opposite). This ‘step-and-shoot’
technologies should be used to
should only be used in
acquisition generates axial slices
permit the deletion of data from
specifically selected cases.
during sequential cycles which are
premature ventricular beats, the
then combined to create the final
insertion of undetected R peaks,
volume. Scanners with wide
and the shifting of R peaks to
detector arrays (up to 160 mm in
adjust for arrhythmia during
the Z-axis) have the potential
retrospective gating.21
to image the entire heart
The potentially high radiation dose
prospectively in a single heart
of retrospective gating can be
beat; this enables scanning of
minimised with dose modulation.22
patients with arrhythmias (including
This is where the radiation dose is
atrial fibrillation [AF]) with no
reduced significantly in parts of the
misregistration artefacts.19
cardiac cycle where there is likely to
Prospective ECG gating should be
be significant cardiac motion, such
the firstline default technique, used
as during systole, and increased to
whenever possible and practical as
diagnostic levels during mid-to-late
it permits a considerable reduction
diastole (Figure 1B, opposite). With
in radiation dose without reduction
the exception of cases where there
in image quality.20
is significant heart rate variability
Where the heart rate exceeds the
(such as atrial fibrillation), dose
recommended threshold for
modulation techniques should be
standard prospective gating,
used with the narrowest selectable
additional tube-on time may be
window of diagnostic tube
used, a technique known as
current.23
‘padding’ (Figure 1D, opposite).
This allows a greater proportion of
the cardiac cycle to be imaged and,
although this means a higher
radiation dose than with standard
prospective gating, it should be
used in preference to retrospective
gating where possible.
Standards of practice of computed tomography
11
coronary angiography (CTCA) in adult patients
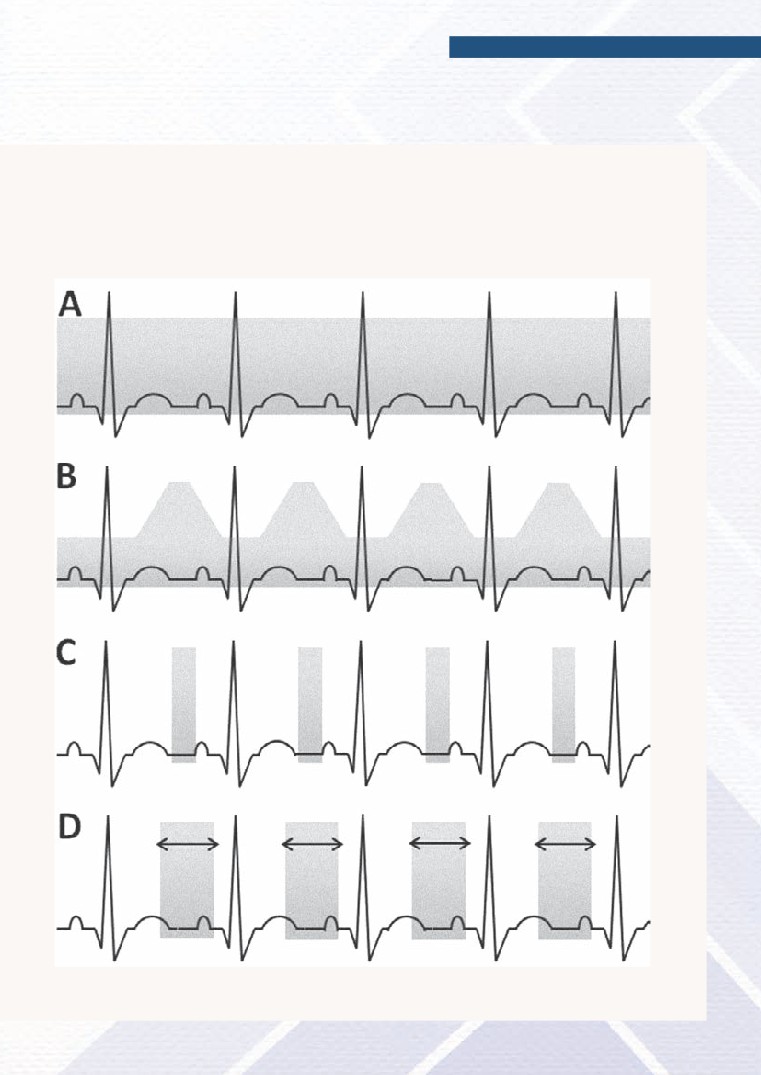
Figure 1. ECG gating techniques
The grey bar represents diagnostic levels of radiation. A = retrospective gating; B = retrospective gating with
dose modulation; C = prospective gating; D = prospective gating with padding. During ‘step-and-shoot’
prospective gating (C and D), the radiation is delivered on alternate or every third heart beat according to the
patient’s heart rate, as the scanner moves or ‘steps’ to the next image position during subsequent heart beats.

Standards of practice of computed tomography
12
coronary angiography (CTCA) in adult patients
Both the reconstruction kernel and
• Where possible, prospective
9. Image quality
slice thickness affect image noise.
ECG gating should be used.
and radiation dose
If the slice thickness is reduced from
• In specifically selected cases
optimisation
1.2 to 0.6 mm, image noise will
where retrospective ECG gating
increase because image noise is
The objective is to obtain
is required, mA modulation
inversely proportional to the square
diagnostic-quality images while
techniques should be used to
root of the slice thickness. To
delivering the lowest reasonably
keep the radiation dose as low
compensate, mAs can be doubled,
achievable radiation dose to the
as possible.
but this, in turn, will double the
patient. Image quality and radiation
patient’s dose of radiation. In
• The scan range should be
dose are intrinsically linked.
practice, a more modest increase in
tailored to each patient. If
Setting the image quality
mAs is often sufficient because the
possible, the scan range must
superior spatial resolution of thin
be set inferior to the shoulders to
Temporal resolution is optimised by
slices compensates for the increase
avoid the prescribed mAs being
using the lowest gantry rotation
in image noise. To optimise spatial
set for the width of the shoulders
time available - typically 350 ms or
resolution in CTCA, a slice thickness
rather than the thorax. The
less. Dual-source scanners have
of less than 1 mm is required, and
greater the detector coverage,
intrinsically better temporal
high-resolution mode should be
the harder it is to tailor the scan
resolution than single-source
considered.
range to the patient’s anatomy.
scanners, without any impact on
In retrospective ECG-gated
patient dose, because the
Contrast resolution is determined
CTCA, the irradiated length may
necessary projections are acquired
by the iodine concentration in the
be up to 60 mm longer than the
in half the scan time than for a
coronary arteries, the tube voltage
imaged length due to helical
single-source scanner. Multiphase
setting and the image noise. The
over-ranging. Adaptive collimators
reconstructions incur a dose
sensitivity to iodine is higher at
will reduce the amount of
penalty over single cardiac phase
lower tube voltages, so 80 or 100
over-ranging present.
ones because they require
kVp are preferable for CTCA. If the
projection data to be acquired over
tube voltage is reduced without
• Scan protocols should be
a longer part of the cardiac cycle.
changing the mAs, the dose to the
size-specific. This is achievable
Multi-segment reconstructions
patient will drop, but image noise
by activating tube current
incur a dose penalty over single-
will increase. Lower energy X-ray
modulation with patient size, or
segment ones because they require
beams may fail to penetrate
setting mAs according to patient
projection data to be acquired
through the anatomy of medium
weight or BMI.
using retrospective ECG gating,
and large patients, leading to streak
• The tube voltage should be
whereas single-segment
artefacts. The optimum choice of
routinely reduced to 100 kVp
reconstructions can be generated
tube voltage is therefore a
for small and medium patients;
from data using prospectively
compromise dependent on the size
iodine contrast agent is more
gated acquisitions which are
of the patient.
conspicuous at lower tube
generally more dose-efficient.
Setting scan protocol parameters
voltages. The mAs can be
Spatial resolution is determined
to optimise the radiation dose
increased modestly to
by the reconstruction kernel and
compensate for the increase
• The displayed predicted
the slice thickness. It is also affected
in image noise. (The prescribed
computed tomography dosage
by the data sampling density
CTDIvol should still be lower at 100
indicatorvol (CTDIvol ) can be used
(which, on some scanners, can
kVp than at 120 kVp.) For very
to monitor how patient dose
be changed by toggling between
small patients, 80 kV can be
might change when scan
normal- and high-resolution modes)
used, with 120 kV used only in
parameters are varied. The
and to a lesser extent by the
large patients.
displayed dose length product
reconstruction field of view.
(DLP) also includes the effect of
• Iterative reconstruction should be
scan range.
critically considered if it can be
built into the CTCA protocol.

Standards of practice of computed tomography
13
coronary angiography (CTCA) in adult patients
Auditing patient doses
Although greater intracoronary
10. The use of
attenuation during CTCA leads to
The DLP is the standard radiation
iodinated contrast
higher diagnostic accuracy in
dose measure used in CTCA.
medium in CTCA
evaluating stenosis, very high
Estimation of effective dose
degrees of enhancement may mean
A 20-gauge or larger right
introduces additional uncertainties
the density of contrast overlaps that
antecubital IV catheter is the
and is not necessary for the
of coronary artery calcium, which
preferred administration route for
purpose of optimisation. The DLPs
can obscure calcified plaques.
iodinated contrast for CTCA. To
used in the department should be
minimise the risk of contrast
subject to regular internal audit and
Contrast infusion rates typically
extravasations, all catheters should
benchmarked against those of
used for CTCA are higher than for
first be tested with a rapidly
other UK centres. The BSCI has
general CT (up to 7.0 ml/s). The
injected bolus of sterile saline to
established a national departmental
ideal situation is for maximal
ensure that the venous access is
radiation dose audit for CTCA, and
contrast enhancement in the
secure and effective. A right arm
CT departments should consider
ascending aorta and the left
cannula is preferable to avoid
submitting radiation dose data to
ventricle and little or no contrast in
artifacts from undiluted contrast
allow benchmarking. A more
the right side of the heart. A saline
media in the left brachiocephalic
detailed list of data that should be
chaser infusion is usually used
vein where it crosses the midline.
collected in addition to DLP levels is
immediately following the contrast
given in Appendix 7.
To obtain optimal diagnostic
medium injection through a
accuracy in CTCA, it is essential that
dual-head power injector at the
References
coronary artery contrast
same rate as the contrast injection;
Further recommended reading on
this can decrease streak artifacts in
enhancement is homogenous and
this topic can be found in
the superior vena cava and
constant throughout the entire scan
references 23, 26 and 27.
maximise the effect of the contrast
range. In addition, the contrast
enhancement should be sufficiently
dose by flushing contrast out of the
intense to allow visualisation of
arm veins. Some centres prefer a
small vessels but not so intense
mixture of contrast and saline to
Standard 7
that it causes beam hardening
follow the pure contrast bolus which
The radiation dose
leads to increased right heart
artefact. The contrast medium
administered should be as low
opacification, allowing a better
infusion protocol for CTCA
as possible, commensurate
assessment of the right heart
therefore needs to be adjusted for
with diagnostic image quality.
structures.
each patient group.
Radiation doses and image
The length of time for which this
Major factors that determine the
quality should be routinely
opacification is required will be
intensity and homogeneity of
and regularly audited and
dependent on scan coverage and
contrast enhancement in the
benchmarked against other
the time taken to scan (which will be
coronary arteries are BMI, cardiac
national centres (Appendix 7).
scanner-specific) so it is vital that
output, the iodine dose and the
the contrast protocol is tailored to
rate at which contrast medium (CM)
the clinical question. For example,
is injected.28-31 The ideal iodine
imaging a patient that has had
delivery rate is between 1-2 g/s
previous coronary artery bypass
depending on the kVp used.32
graft surgery means that a 25%
increase in contrast volume will
typically be required as the scan will
need to start from the level of the
internal mammary artery origin.

Standards of practice of computed tomography
14
coronary angiography (CTCA) in adult patients
Intravascular contrast attenuation
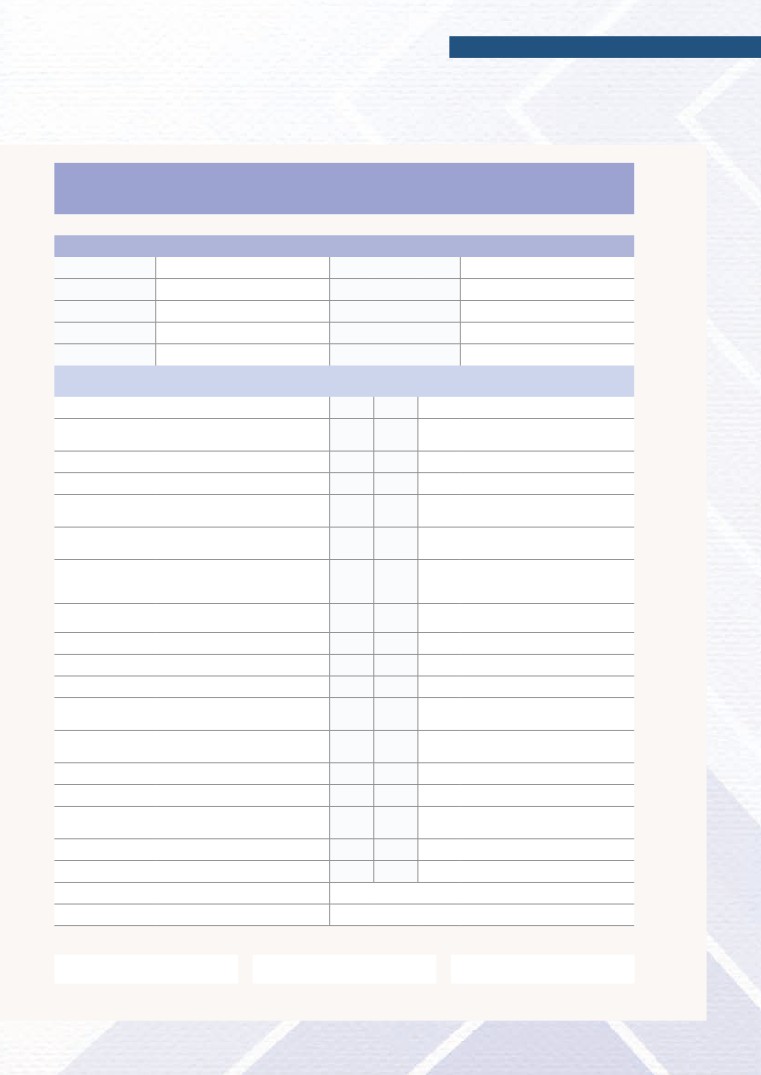
Table 1. Potential contrast protocol for a 64-slice CT scanner using
can be optimised by decreasing the
a contrast concentration of 350 mgI/ml
tube voltage (to 100 or 80 kVp)
kVp
Flow rate
Contrast volume
Saline volume
which increases the opacification of
(ml/s)
(ml/s)
(ml/s)
the blood vessels because of an
increase in the X-ray absorption of
80
3.5
60
25
iodine at lower photon energies.
100
5.0
75
35
This will also decrease radiation
dose if the tube current is kept
120
6.5
95
50
constant. However, this will increase
140
7.0
100
60
image noise which may mitigate the
effect of the increased vascular
opacification. If image noise is kept
constant by increasing the tube
Timing of the scan acquisition
current, it is possible to produce
Standard 8
following contrast injection
equivalent image quality and
The iodinated contrast
contrast opacification with
Due to substantial variations in the
medium delivery protocol
equivalent radiation dose,
time required for the IV contrast
should be adjusted for each
compared with higher kVp
injection to reach the targeted
patient group and according
techniques using lower doses of IV
vascular anatomy, an assessment of
to the scanner being used.
contrast medium. This reduction in
patient-specific circulation time is
contrast dose reduces the risk of
required. Circulation timing can be
nephrotoxicity and can allow
performed using two techniques:
substantial cost savings.29 Due to
the test bolus technique (using
the fact that lower tube voltages
10-15 ml of contrast medium at the
produce fewer photons (for a given
same flow rate and via the IV site to
mA), low kVp scanning is not
be used during the CTCA
possible in very obese patients.
acquisition) or the bolus tracking
and trigger technique. The choice
Contrast protocols
of technique is a matter of personal
Providing precise recommendations
operator or unit preference and is
on contrast regimens which cover
also dependent on the scanner
all clinical scenarios and CT scanner
technology used.
types is very difficult. However, a
typical example of injection flow
rates for CTCA using a 64-slice CT
system for coronary artery imaging
is given in Table 1 (assuming a
contrast concentration of
350 mgI/ml). Contrast volumes are
typically lower with CT scanners
capable of single heart beat
acquisition (either wide-area
detector or high pitch dual-tube
scanners).
Standards of practice of computed tomography
15
coronary angiography (CTCA) in adult patients
The department should take the
11. Patient care during
opportunity to capture periodically
and after the scan
formal feedback from patients on
The patient’s heart rate and rhythm
their opinions of the experience of
should be monitored continuously
the procedure. This may take the
via the ECG on the scanner console.
form of a patient-satisfaction survey
or a patient-experience
Immediately before the scan starts,
questionnaire. Examples of these
the breath-hold requirements of the
are available on the RCR website
scan should be explained to the
patient together with common
feedback should be routinely
expected sensations caused by the
reviewed and discussed as part of a
intravenous contrast medium.
regular service evaluation, together
Once the scan has been completed,
with a review of cases with
the patient should be warned that
complications and cases of ‘near-
they may experience light-
miss’ incidents. This will help the
headedness on sitting up and
department to refine protocols and
getting off the scanner table,
continue staff training to ensure
particularly if beta-blockers have
high-quality and safe patient care.
been administered. A member of
staff should be with the patient as
they get off the scanner table
and should escort them to the
Standard 9
changing room.
The patient should be
The length of time the patient
reviewed by an appropriately
remains in the imaging department
qualified member of staff
after the scan is a matter of local
prior to discharge from the
choice, but will depend on the
scanning department.
presence of patient symptoms
related to the drugs or contrast
medium administered. Current RCR
guidelines for patients undergoing
a contrast-enhanced CT scan state
Approved by The Royal College of
that the patient should wait in the
Radiologists Clinical Radiology Faculty
department for 15 minutes before
Board: 27 June 2014.
leaving, or 30 minutes if there is an
Approved by the British Society of
increased risk of contrast reaction. If
Cardiovascular Imaging: 18 June 2014
the patient has persisting
Approved by the Royal College of
symptoms relating to heart rate-
Physicians: 8 July 2014
controlling medication, they should
remain monitored in the
department until these resolve;
advice and review from the on-call
cardiology or general medicine
team may be required.

Standards of practice of computed tomography
16
coronary angiography (CTCA) in adult patients
9.
Raju VM, Gosling OE, Morgan-Hughes
15.
Health and Safety Executive.
References
G et al. High-dose intravenous
Ionising Radiation Regulations 1999.
1.
The Mid Staffordshire NHS
metoprolol usage for reducing heart
London: The Stationery Office, 1999.
Foundation Trust Public Inquiry.
rate at CT coronary angiography:
Chaired by Robert Francis QC.
efficacy and safety. Clin Radiol 2014;
16.
Department of Health. Cardiac
Report of the Mid Staffordshire NHS
69(7): 739-744.
imaging - A report from the national
Foundation Trust Public Inquiry.
imaging board. London: Department
London: The Stationery Office, 2013.
10.
Roberts WT, Wright AR, Timmis JB,
of Health, 2010.
Timmis AD. Safety and efficacy of a
2.
rate control protocol for cardiac CT.
17.
National Institute of Health and Care
28/10/2014)
Br J Radiol 2009; 82(976): 267-271.
Excellence. Chest pain of recent onset:
assessment and diagnosis of recent
3.
11.
Guaricci AI, Schuijf JD, Cademartiri F
onset chest pain or discomfort of
28/10/2014)
et al. Incremental value and safety of
suspected cardiac origin. NICE Clinical
oral ivabradine for heart rate reduction
Guidelines, No. 95. London: National
4.
Raff GL, Abidov A, Achenbach S et al.
in computed tomography coronary
Institute of Health and Care
SCCT guidelines for the interpretation
angiography. Int J Cardiol 2012;
Excellence, 2010.
and reporting of coronary computed
156(1): 28-33.
tomographic angiography.
18.
American College of Cardiology
J Cardiovasc Comput Tomogr 2009;
12.
Abbara S, Arbab-Zadeh A, Callister
Foundation Task Force on Expert
3(2): 122-136.
TQ et al. SCCT guidelines for
Consensus Documents. ACCF/ACR/
performance of coronary computed
AHA/NASCI/SAIP/SCAI/SCCT 2010
5.
Health and Safety Executive.
tomographic angiography: a report of
expert consensus document on
Ionising Radiation (Medical Exposure)
the Society of Cardiovascular
coronary computed tomographic
Regulations 2000. London:
Computed Tomography Guidelines
angiography: a report of the American
The Stationery Office, 2000.
Committee. J Cardiovasc Comput
College of Cardiology Foundation
Tomogr 2009; 3(3): 190-204.
Task Force on Expert Consensus
Documents. J Am Coll Cardiol 2010;
6.
Achenbach S, Manolopoulos M,
55(23): 2663-2699.
Schuhbäck A et al. Influence of heart
13.
The Royal College of Radiologists.
rate and phase of the cardiac cycle on
Standards for intravascular contrast
the occurrence of motion artifact in
agent administration to adult patients,
19.
Halliburton S, Arbab-Zadeh A,
dual-source CT angiography of the
Second edition. London: The Royal
Dey D et al. State-of-the-art in CT
coronary arteries. J Cardiovasc
College of Radiologists, 2010.
hardware and scan modes for
Comput Tomogr 2012; 6(2): 91-98.
cardiovascular CT. J Cardiovasc
Comput Tomogr 2012; 6(3): 154-163.
14.
National Institute for Health and
7.
Care Excellence. New generation
current/2-cardiovascular-system/
cardiac CT scanners (Aquilion ONE,
20.
Sun Z, Ng KH. Prospective versus
24-beta-adrenoceptor-blocking-
Brilliance iCT, Discovery CT750 HD and
retrospective ECG-gated multislice
drugs/metoprolol-tartrate (last
Somatom Definition Flash) for cardiac
CT coronary angiography:
accessed 28/10/2014)
imaging in people with suspected or
a systematic review of radiation dose
known coronary artery disease in
and diagnostic accuracy. Eur J Radiol
whom imaging is difficult with earlier
2012; 81(2): e94-e100.
8.
Shapiro MD, Pena AJ, Nichols JH et al.
generation CT scanners (Diagnostics
Efficacy of pre-scan beta-blockade
Guidance 3). London: National
and impact of heart rate on image
21.
Cademartiri F, Mollet NR, Runza G
Institute for Health and Care
quality in patients undergoing
et al. Improving diagnostic accuracy
Excellence, 2012.
coronary multidetector computed
of MDCT coronary angiography in
tomography angiography. Eur J Radiol
patients with mild heart rhythm
2008; 66(1): 37-41.
irregularities using ECG editing.
AJR Am J Roentgenol 2006; 186(3):
634-638.

Standards of practice of computed tomography
17
coronary angiography (CTCA) in adult patients
22.
Gosling O, Loader R, Venables P et al.
29.
Setty BN, Sahani DV, Ouellette-
A comparison of radiation doses
Piazzo K, Hahn PF, Shepard JA.
between state-of-the-art multislice CT
Comparison of enhancement,
coronary angiography with iterative
image quality, cost, and adverse
reconstruction, multislice CT coronary
reactions using 2 different
angiography with standard filtered
contrast medium concentrations
back-projection and invasive
for routine chest CT on 16-slice
diagnostic coronary angiography.
MDCT. J Comput Assist Tomogr
Heart 2010; 96(12): 922-926.
2006; 30(5): 818-822.
23.
Halliburton SS, Abbara S, Chen MY et
30.
Husmann L, Alkadhi H, Boehm T
al. SCCT guidelines on radiation dose
et al. Influence of cardiac
and dose-optimization strategies in
hemodynamic parameters on
cardiovascular CT. J Cardiovasc
coronary artery opacification with
Comput Tomogr 2011; 5(4): 198-224.
64-slice computed tomography.
Eur Radiol 2006; 16(5): 1111-1116.
24.
Achenbach S, Marwan M, Schepis T
et al. High-pitch spiral acquisition:
31.
Husmann L, Leschka S, Boehm T
a new scan mode for coronary CT
et al. Influence of body mass index
angiography. J Cardiovasc Comput
on coronary artery opacification in
Tomogr 2009; 3(2): 117-121.
64-slice CT angiography. Rofo
2006; 178(10): 1007-1013.
25.
Achenbach S, Marwan M, Ropers D
et al. Coronary computed tomography
32.
Rutten A, Meijs MF, de Vos AM,
angiography with a consistent dose
Seidensticker PR, Prokop M.
below 1 mSv using prospectively
Biphasic contrast medium
electrocardiogram-triggered
injection in cardiac CT: moderate
high-pitch spiral acquisition. Eur Heart
versus high concentration contrast
J 2010; 31(3): 340-346.
material at identical iodine flux
and iodine dose. Eur Radiol 2010;
20(8): 1917-1925.
26.
Mayo JR, Leipsic JA. Radiation
dose in cardiac CT. AJR Am J
Roentgenol 2009; 192(3): 646-653.
33.
accessed 28/10/2014)
27.
Roobottom CA, Mitchell G,
Morgan-Hughes G. Radiation-
reduction strategies in cardiac
computed tomographic
angiography. Clin Radiol 2010;
65(11): 859-867.
28.
Fleischmann D. Present and future
trends in multiple detector-row CT
applications: CT angiography. Eur
Radiol 2002; 12(2): S11-S15.

Standards of practice of computed tomography
18
coronary angiography (CTCA) in adult patients
Appendix 1. Contributing authors and reviewers
Working party
Dr Stephen Harden, Consultant radiologist, Southampton (Chair)
Dr Russell Bull, Consultant radiologist, Bournemouth
Dr Roger Bury, Consultant radiologist, Blackpool
Dr Elly Castellano, CT radiation physicist, Royal Marsden Hospital, London
Dr Mark Hamilton, Consultant radiologist, Bristol
Dr Gareth Morgan-Hughes, Consultant cardiologist, Plymouth, (RCP representative)
Dr Ed Nicol, Consultant cardiologist, Royal Brompton Hospital, London
Dr Giles Roditi, Consultant radiologist, Glasgow
Prof Carl Roobottom, Consultant radiologist, Plymouth
Dr Simon Padley, Consultant radiologist, Royal Brompton Hospital, London
Dr Jim Stirrup, Cardiology registrar, Southampton
Dr Robert Thurstans, Patient liaison representative
Dr Raman Uberoi, Consultant radiologist, Oxford, (RCR PSSB representative)
Other contributing authors and section reviewers
Ms Rachel Bradford, Senior CT radiographer, Southampton
Dr Ben Clayton, Cardiology registrar, Plymouth
Dr Ceri Davies, Consultant cardiologist, London Chest Hospital
Dr Mark Kon, Consultant radiologist, Bradford
Dr Robert Loader, Clinical scientist, Plymouth
Dr Declan O’Regan, Consultant radiologist, Hammersmith Hospital, London
Dr Francesca Pugliese, Consultant radiologist, London Chest Hospital
Dr James Shambrook, Consultant radiologist, Southampton
Dr Tricia Woodhead, Consultant radiologist, Weston (RCR Patient Safety Adviser)
Standards of practice of computed tomography
19
coronary angiography (CTCA) in adult patients
Standards of practice of computed tomography
20
coronary angiography (CTCA) in adult patients
Standards of practice of computed tomography
21
coronary angiography (CTCA) in adult patients
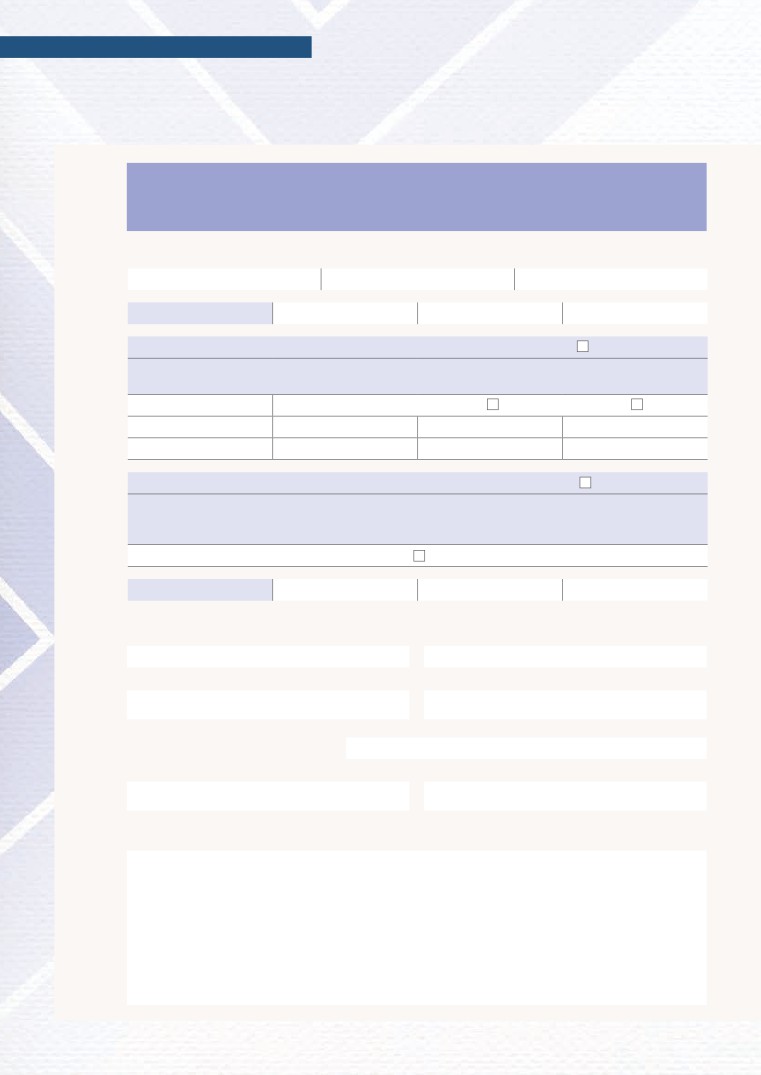
Appendix 3. CTCA patient safety questionnaire
Patient details
Date
Patient name
Radiologist
Hospital ID
Radiographer
Date of birth
Nurse
Last menstrual period
Height
Weight
Pre-procedure checklist (to be completed by
If yes:
radiographer or nurse)
Have you had a previous severe allergic reaction?
Yes
No
Discuss with radiologist.
Have you had a reaction to contrast medium
Yes
No
(X-ray dye) in the past?
Do you have asthma?
Yes
No
If yes, do you use an inhaler?
Yes
No
Are you currently wheezy or is the asthma poorly
Yes
No
Do not give beta-blockers.
controlled?
Have you taken Viagra (sildenafil) within the last
Yes
No
Do not give glyceryl trinitrate (GTN).
24 hours?
Do you have a history of heart disease such as heart
Yes
No
Do not give GTN if severe aortic stenosis.
failure, heart block, heart valve disease or a family
Do not give beta-blockers if heart failure
history of heart disease?
or 2nd/3rd degree heart block.
Are you taking verapamil?
Yes
No
Do not give beta-blockers.
Do you have diabetes?
Yes
No
Do you take metformin?
Yes
No
Check recent urea and electrocytes (U+E).
Do you have or have you had high blood pressure?
Yes
No
Do you have kidney problems, kidney failure or have
Yes
No
you ever been on dialysis? If so please specify.
Do you have gout, liver disease, myeloma or peripheral
Yes
No
vascular disease?
Have you had heart surgery or stents inserted?
Yes
No
Do you have a pacemaker or implantable defibrillator?
Yes
No
Do you consent to the use of your CT images for
Yes
No
research, audit or teaching?
For female patients: Could you be pregnant?
Yes
No
Are you breast feeding?
Yes
No
Medications
Allergies
Print name:
Patient’s signature:
Date:

Standards of practice of computed tomography
22
coronary angiography (CTCA) in adult patients
Both metoprolol and atenolol have
Appendix 4.
similar half-lives (up to seven hours),
Pharmacokinetics of
although renal dysfunction increases
beta-blockers used for
the half-life of atenolol (>27 hrs if
heart rate reduction
estimated glomerular filtration rate
(eGFR) <15 ml/kg/1.73 m2). The half-life
prior to CTCA
of metoprolol is unaffected by renal
Beta-blockers work by diminishing
function as it is metabolised almost
sympathetic activation of the heart,
exclusively by the liver.
decreasing heart rate and myocardial
Esmolol has also been used for heart
contractility. The available beta-
control prior to CTCA. It is a
blockers differ in their cardioselectivity
cardioselective beta-1 adrenoceptor
although this is relative and
antagonist with an extremely short
dependent on dose: the higher the
half-life (nine minutes) but is available
dose used, the less cardioselective
only as an IV preparation.
the beta-blocker. Blockade of beta-1
adrenoceptors leads to reduction in
The effects of beta-blockers may be
heart rate and contractility; beta-2
potentiated when administered in
adrenoceptors are found in bronchial
patients on other long-term rate-
smooth muscle and cause
controlling agents (calcium channel
bronchoconstriction when inhibited. It
blockers, digoxin, amiodarone). The
is therefore preferable to use beta-1
effects of metoprolol and propanolol
selective adrenoceptor antagonists in
in particular may be potentiated when
the setting of heart rate control.
co-administered with inhibitors of
cytochrome P450, such as fluoxetine,
The most commonly used beta-
paroxetine, propafenone, quinidine,
blocker prior to CTCA in the UK is
sertraline and amiodarone. However,
metoprolol. There is some usage of
these are unlikely to cause issues for
atenolol, with 100 mg given orally one
short-term beta-blocker dosing used
hour before the scan; IV atenolol is
in CTCA.
used infrequently in the UK. Given the
higher lipid solubility of metoprolol,
peak plasma concentrations after oral
ingestion are achieved more quickly
(90 minutes versus 120-240 minutes
with atenolol), with an effect on
systolic blood pressure seen within
15 minutes. In contrast, peak plasma
levels are seen usually within five
minutes when given intravenously.
Standards of practice of computed tomography
23
coronary angiography (CTCA) in adult patients
Appendix 5. Treatment of adverse events after heart
rate-lowering medication
Seek assistance from clinician covering the scan session if the patient experiences:
Bradycardia
• Heart rate <40 bpm or <50 bpm and symptomatic
• Atropine 600 mcg IV every 2-3 minutes up to a maximum of 2,400 mcg
• If persistent and following beta-blockade/calcium channel blockade: administer 50 mcg/kg IV glucagon
(one vial mixed with 5% dextrose)
• Bleep on-call cardiology/general medical specialty registrar (StR).
Hypotension
• If it is in the setting of bradycardia, treat as above
• Otherwise, give 250 mL 0.9% sodium chloride (‘normal saline’) IV bolus
• Bleep on-call cardiology/general medical StR.
Cardiac arrest
• Call for help
• Start basic life support in accordance with published guidelines
• A second staff member should dial the cardiac arrest team giving location (CT scanner, building x, level x) a
nd nature of emergency (adult cardiac arrest), and bring the resuscitation trolley.
Standards of practice of computed tomography
24
coronary angiography (CTCA) in adult patients
Appendix 6. Monitoring checklist for adult patients receiving
beta-blockers for lowering heart rate +/- sublingual GTN for CTCA
Prescriptions and observations
Time
HR
BP
Baseline observations
ß-Blockers Contraindications (C/I) and cautions checked?
C/I - Hypotension (BP <90/60 mmHg), asthma (bronchospasm), severe peripheral vascular disease, severe aortic
stenosis, uncontrolled heart failure, sick sinus syndrome, 2nd/3rd degree heart block, on verapamil
Agent
Metoprolol 50-100 mg po
Metoprolol 5-30 mg IV
Dose
mg
Dose
mg
Glyceryl trintrate Contraindications and cautions checked?
C/I - Hypersensitivity to nitrates, hypotension (BP <90/60 mmHg), use of Viagra, Cialis or Levitra within last 24
hours, hypertrophic cardiomyopathy, aortic stenosis, cardiac tamponade, constrictive pericarditis, mitral
stenosis, known severe anaemia
400-800 mcg sublingually just prior to CT scan
Discharge observations
Drugs prescribed by:
Given by:
Signature:
Signature:
Time patient discharged from department:
Print name:
Signature:
Notes:

Standards of practice of computed tomography
25
coronary angiography (CTCA) in adult patients
• Dose indicators for the standard
Appendix 7. Auditing
70 kg subject are calculated
patient radiation doses
as follows.
in CTCA
- Data for patients with weight in
Beta-DLP data can be easily obtained
the range 60-80 kg or a BMI of
by interrogating the radiology
20-30 can be selected. Patients
information system. Unfortunately, the
undergoing CTCA are typically
data is of limited use for
heavier than the general
benchmarking and optimising scan
population, so the average patient
protocols. A more detailed dose audit
may be closer to 80 kg than 70 kg
which collects CTCA patient
in weight. It may therefore be
demographics and heart rate
more appropriate to select data in
characteristics is necessary. The
the range 70-90 kg but this
department’s medical physics expert
remains to be determined.
should be involved for best results.
- The median CTDIvol and DLP for
The recommended data required for
each series and the median
each patient for CTCA dose audit is
examination DLP are calculated
as follows.
for each type of scan protocol in
• A sample of at least 60 examinations
clinical use and, if there is sufficient
is desirable, including:
data, for slow, medium and fast
heart rates.
- Patient demographics
(sex, weight or BMI)
• The dose distribution for the patient
population is calculated as follows.
- Previous ischaemic heart disease
(coronary artery bypass grafting
- Data for each type of scan
[CABG], stents)
protocol in clinical use is selected.
- Acquisition heart rate and heart
- CTDIvol and DLP are plotted
rate variability
against patient size (weight or BMI)
and heart rate. The variation of
- Scan protocol selected
with patient size and heart
CTDIvol
- Cardiac phases imaged
rate provides an insight into how
- CTDIvol and DLP for each
the tube current prescription
scan series
(manual or automatic) varies with
these parameters.
- Total DLP.
- It may be possible to fit a
polynomial curve to the data to
predict the CTDIvol and DLP
for subjects of other sizes and
heart rates.

Citation details
The Royal College of Physicians, the British Society
For permission to reproduce any of the content
of Cardiovascular Imaging and The Royal College
contained herein, please email: permissions@rcr.ac.uk
of Radiologists. Standards of practice of computed
tomography coronary angiography (CTCA) in
This material has been produced by The Royal
adult patients. London: The Royal College of
College of Physicians, the British Society of
Radiologists, 2014.
Cardiovascular Imaging and The Royal College
of Radiologists (RCR) for use internally within the
Ref No. BFCR(14)16
specialties of clinical cardiology and clinical radiology
© The Royal College of Radiologists, December 2014.
in the United Kingdom. It is provided for use by
appropriately qualified professionals, and the making
of any decision regarding the applicability and
suitability of the material in any particular circumstance
is subject to the user’s professional judgement.
While every reasonable care has been taken to ensure
the accuracy of the material, RCR cannot accept any
responsibility for any action taken, or not taken, on
The Royal College of Radiologists
the basis of it. As publisher, RCR shall not be liable to
63 Lincoln’s Inn Fields, London WC2A 3JW
any person for any loss or damage, which may arise
Tel: +44 (0)20 7405 1282
from the use of any of the material. The RCR does not
exclude or limit liability for death or personal injury to
Email: enquiries@rcr.ac.uk www.rcr.ac.uk
the extent only that the same arises as a result of the
negligence of RCR, its employees, Officers, members
A Charity registered with the
and Fellows, or any other person contributing to the
Charity Commission No. 211540
formulation of the material.