
Coronary Computed Tomography Angiography With Selective
Noninvasive Fractional Flow Reserve
Policy #
00537
Original Effective Date:
02/15/2017
Current Effective Date:
10/18/2017
Applies to all products administered or underwritten by Blue Cross and Blue Shield of Louisiana and its subsidiary, HMO Louisiana,
Inc.(collectively referred to as the “Company”), unless otherwise provided in the applicable contract. Medical technology is constantly
evolving, and we reserve the right to review and update Medical Policy periodically.
Note: Contrast-Enhanced Coronary Computed Tomography Angiography (CCTA) for Coronary Artery
Evaluation is addressed in medical policy 00153.
Note: Positron Emission Tomography (PET) Cardiac Applications is addressed in medical policy 00103.
When Services Are Eligible for Coverage
Coverage for eligible medical treatments or procedures, drugs, devices or biological products may be
provided only if:
• Benefits are available in the member’s contract/certificate, and
• Medical necessity criteria and guidelines are met.
Based on review of available data, the Company may consider the use of noninvasive fractional flow
reserve (FFR) following a positive coronary computed tomography angiography (CCTA) to guide decisions
about the use of invasive coronary angiography (ICA) in patients with stable chest pain at intermediate risk
of coronary artery disease (CAD i.e., suspected or presumed stable ischemic heart disease [SIHD]) to be
eligible for coverage.
When Services Are Considered Investigational
Coverage is not available for investigational medical treatments or procedures, drugs, devices or biological
products.
The use of noninvasive fractional flow reserve (FFR) not meeting the criteria outlined above is considered to
be investigational.*
Background/Overview
STABLE ISCHEMIC HEART DISEASE
CAD is a significant cause of morbidity and mortality and various epidemiologic risk factors have been well
studied. Evaluation of obstructive CAD involves quantifying arterial stenoses to determine whether
significant narrowing is present. Lesions with stenosis more than 50% to 70% in diameter accompanied by
symptoms are generally considered significant. It has been suggested that CCTA or other noninvasive
functional cardiac testing may help rule out CAD and avoid ICA in patients with a low clinical likelihood of
significant CAD. However, ICAs are frequently unnecessary in patients with suspected SIHD, as evidenced
by low diagnostic yields for significant obstructive CAD. For example, from a sample of over 132,000 ICAs,
Patel et al (2010) found 48.8% of elective ICAs performed in patients with stable angina did not detect
obstructive CAD (left main stenosis ≥50% or ≥70% in a major epicardial or branch >2.0 mm in diameter).
ICA is clinically useful when patients with stable angina have failed optimal medical therapy (OMT) and may
©2017 Blue Cross and Blue Shield of Louisiana
Blue Cross and Blue Shield of Louisiana is an independent licensee of the Blue Cross and Blue Shield Association and incorporated
as Louisiana Health Service & Indemnity Company.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic,
mechanical, photocopying, or otherwise, without permission from Blue Cross and Blue Shield of Louisiana.
Page 1 of 21

Coronary Computed Tomography Angiography With Selective Noninvasive Fractional Flow Reserve
Policy #
00537
Original Effective Date:
02/15/2017
Current Effective Date:
10/18/2017
benefit from revascularization. A noninvasive imaging test, performed prior to ICA as a gatekeeper, that can
distinguish candidates who may benefit from early revascularization (e.g., patients with unprotected left
main stenosis ≥50% or hemodynamically significant disease) from those unlikely to benefit could avoid
unnecessary invasive procedures and their potential adverse consequences. Moreover, for the large
majority of patients with SIHD, revascularization offers no survival advantage over medical therapy; there
are few who might benefit from ICA if they have not first failed OMT.
Clinical Risk Prediction
The 2012 collaborative medical association guidelines for the diagnosis and management of patients with
stable heart disease list several class I recommendations on use of noninvasive testing in patients with
suspected SIHD. A class I recommendation indicates that a test should be performed. In general, patients
with at least intermediate risk (10%-90% risk by standard risk prediction instruments) are recommended to
have some type of test, the choice depending on interpretability of the electrocardiogram, capacity to
exercise, and presence of comorbidity.
Clinical prediction scores or models have been developed to help estimate the pretest probability of CAD in
individuals with stable chest pain. A commonly cited clinical prediction model based on age, sex, and type
of pain symptoms, originally developed by Diamond and Forrester (1979), has been further studied and
extended in a report by Genders et al (2011) and compared to the Duke Clinical Score by Wasfy et al
(2012). Versteylen et al (2011) published a comparison of clinical prediction results for the Diamond and
Forrester model, the Framingham risk score, the PROCAM risk score, and the SCORE risk estimation
model. Another model has been published by Min et al (2015) and an online calculator developed by a CAD
consortium.
Gatekeepers to ICA
Imposing an effective noninvasive gatekeeper strategy with one or more tests before planned ICA to avoid
unnecessary procedures is compelling. The most important characteristic of a gatekeeper test is its ability to
accurately identify and exclude clinically insignificant disease where revascularization would offer no
potential benefit. From a diagnostic perspective, an optimal strategy would result in few false-negative tests
while avoiding an excessive false-positive rate—it would provide a low posttest probability of significant
disease. Such a test would then have a small and precise negative likelihood ratio and high negative
predictive value. An effective gatekeeper would decrease the rate of ICA while increasing the diagnostic
yield (defined by the presence of obstructive CAD on ICA). At the same time, there should be no increase in
major adverse cardiac events. A clinically useful strategy would satisfy these diagnostic performance
characteristics and impact the outcomes of interest. Various tests have been proposed as potentially
appropriate for a gatekeeper function prior to planned ICA, including CCTA, magnetic resonance imaging
(MRI), single-photon emission computed tomography (SPECT), positron emission tomography (PET), and
stress echocardiography. More recently, adding noninvasive measurement of fractional flow reserve using
coronary computed tomography angiography (FFR-CT) has been suggested, combining functional and
anatomic information.
©2017 Blue Cross and Blue Shield of Louisiana
Blue Cross and Blue Shield of Louisiana is an independent licensee of the Blue Cross and Blue Shield Association and incorporated
as Louisiana Health Service & Indemnity Company.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic,
mechanical, photocopying, or otherwise, without permission from Blue Cross and Blue Shield of Louisiana.
Page 2 of 21

Coronary Computed Tomography Angiography With Selective Noninvasive Fractional Flow Reserve
Policy #
00537
Original Effective Date:
02/15/2017
Current Effective Date:
10/18/2017
Fractional Flow Reserve
Invasively measured FFR evaluates the severity of ischemia caused by coronary artery obstructions and
can predict when revascularization may be beneficial. FFR has not been used as a diagnostic test for
ischemic heart disease, but as a test to evaluate the degree of ischemia caused by a stenosis.
Invasive FFR is rarely used in the United States to guide percutaneous coronary intervention (PCI). For
example, using the National Inpatient Sample, Pothineni et al (2016) reported that 201,705 PCIs were
performed in 2012, but just 21,365 FFR procedures. Assuming the intention of FFR is to guide PCI, it would
represent just
4.3% of PCI procedures. Whether noninvasively obtained FFR will influence decisions
concerning ICA, over and above anatomic considerations, is therefore important to empirically establish.
Randomized controlled trials and observational studies have demonstrated that FFR-guided
revascularization can improve cardiovascular outcomes, reduce revascularizations, and decrease costs.
For example, the FFR versus Angiography for Multivessel Evaluation (FAME) trial randomized 1005
patients with multivessel disease and planned PCI. At 1 year, compared with PCI guided by angiography
alone, FFR-guided PCI reduced the number of stents placed by approximately 30%—followed by lower
rates (13.2% vs 18.3%) of major cardiovascular adverse events (myocardial infarction [MI], death, repeat
revascularization) and at a lower cost. The clinical benefit persisted through 2 years, although by 5 years
events rates were similar between groups.
European [EU] guidelines (2013) for stable CAD have recommended that FFR be used “to identify
hemodynamically relevant coronary lesion(s) when evidence of ischaemia is not available” (class Ia), and
“[r]evascularization of stenoses with FFR <0.80 is recommended in patients with angina symptoms or a
positive stress test.” Guidelines (2014) have also recommended using “FFR to identify haemodynamically
relevant coronary lesion(s) in stable patients when evidence of ischaemia is not available” (class Ia
recommendation). U.S. guidelines (2012) have stated that an FFR of 0.80 or less provides level Ia evidence
for revascularization for
“significant stenoses amenable to revascularization and unacceptable angina
despite guideline directed medical therapy.” In addition, the importance of FFR in decision making appears
prominently in the 2017 appropriate use criteria for coronary revascularization in patients with SIHD.
Measuring FFR during ICA can be accomplished by passing a pressure-sensing guidewire across a
stenosis. Coronary hyperemia (increased blood flow) is then induced and pressure distal and proximal to
the stenosis is used to calculate flow across it. FFR is the ratio of flow in the presence of a stenosis to flow
in its absence. FFR levels less than 0.75 to 0.80 are considered to represent significant ischemia while
those 0.94 to 1.0 normal. Measurement is valid in the presence of serial stenoses, is unaffected by
collateral blood flow, and reproducibility is high. Potential complications include adverse events related to
catheter use such as vessel wall damage (dissection); the time required to obtain FFR during a typical ICA
is less than 10 minutes.
FFR using CCTA requires at least 64-slice CCTA and cannot be calculated when images lack sufficient
quality (11% to 13% in recent studies), e.g., in obese individuals (e.g., body mass index, >35 kg/m2). The
presence of dense arterial calcification or an intracoronary stent can produce significant beam-hardening
©2017 Blue Cross and Blue Shield of Louisiana
Blue Cross and Blue Shield of Louisiana is an independent licensee of the Blue Cross and Blue Shield Association and incorporated
as Louisiana Health Service & Indemnity Company.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic,
mechanical, photocopying, or otherwise, without permission from Blue Cross and Blue Shield of Louisiana.
Page 3 of 21

Coronary Computed Tomography Angiography With Selective Noninvasive Fractional Flow Reserve
Policy #
00537
Original Effective Date:
02/15/2017
Current Effective Date:
10/18/2017
artifacts and may preclude satisfactory imaging. The presence of an uncontrolled rapid heart rate or
arrhythmia hinders the ability to obtain diagnostically satisfactory images. Evaluation of the distal coronary
arteries is generally more difficult than visualization of the proximal and mid-segment coronary arteries due
to greater cardiac motion and the smaller caliber of coronary vessels in distal locations.
Noninvasive FFR Measurement
FFR can be modeled noninvasively using images obtained during CCTA—so-called FFR-CT (HeartFlow
software termed FFRCT; Siemens cFFR) using routinely collected CCTA imaging data. The process involves
constructing a digital model of coronary anatomy and calculating FFR across the entire vascular tree using
computational fluid dynamics. FFR-CT can also be used for “virtual stenting” to simulate how stent
placement would be predicted to improve vessel flow.
Only the HeartFlow FFRCT software has been cleared by the U.S. Food and Drug Administration (FDA).
Imaging analyses require transmitting data to a central location for analysis, taking 1 to 3 days to complete.
Other prototype software is workstation-based with onsite analyses. FFR-CT requires at least 64-slice
CCTA and cannot be calculated when images lack sufficient quality (11% to 13% in recent studies), e.g., in
obese individuals (e.g., body mass index, >35 kg/m2).
FDA or Other Governmental Regulatory Approval
U.S. Food and Drug Administration
In November 2014, FFRCT simulation software (HeartFlow) was cleared for marketing by the U.S. FDA
through the de novo 510(k) process (class II, special controls; FDA product code: PJA). In January 2016,
the FFRCT v2.0 device was cleared through a subsequent 510(k) process.
HeartFlow FFRCT postprocessing software is cleared “for the clinical quantitative and qualitative analysis of
previously acquired Computed Tomography [CT] DICOM [Digital Imaging and Communications in Medicine]
data for clinically stable symptomatic patients with CAD. It provides FFRCT, a mathematically derived
quantity, computed from simulated pressure, velocity and blood flow information obtained from a 3D
computer model generated from static coronary CT images. FFRCT analysis is intended to support the
functional evaluation of CAD. The results of this analysis [FFRCT] are provided to support qualified clinicians
to aid in the evaluation and assessment of coronary arteries. The results of HeartFlow FFRCT are intended
to be used by qualified clinicians in conjunction with the patient’s clinical history, symptoms, and other
diagnostic tests, as well as the clinician’s professional judgment.”
Centers for Medicare and Medicaid Services (CMS)
There is no national coverage determination (NCD). In the absence of an NCD, coverage decisions are left
to the discretion of local Medicare carriers.
Rationale/Source
The most recent literature review was performed to identify literature assessing the potential impact of
noninvasive imaging, particularly focusing on use of CCTA and noninvasive FFR to guide use of ICA in
©2017 Blue Cross and Blue Shield of Louisiana
Blue Cross and Blue Shield of Louisiana is an independent licensee of the Blue Cross and Blue Shield Association and incorporated
as Louisiana Health Service & Indemnity Company.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic,
mechanical, photocopying, or otherwise, without permission from Blue Cross and Blue Shield of Louisiana.
Page 4 of 21

Coronary Computed Tomography Angiography With Selective Noninvasive Fractional Flow Reserve
Policy #
00537
Original Effective Date:
02/15/2017
Current Effective Date:
10/18/2017
patients with stable chest pain at intermediate risk of CAD (i.e., suspected or presumed SIHD) being
considered for ICA. HeartFlow also submitted a list of publications and materials for review.
Assessment of a diagnostic technology typically focuses on 3 categories of evidence: (1) its technical
performance (test-retest reliability or interrater reliability); (2) diagnostic accuracy (sensitivity, specificity, and
positive and negative predictive value) in relevant populations of patients; and
(3) clinical utility
demonstrating that the diagnostic information can be used to improve patient outcomes.
CCTA WITH SELECTIVE NONINVASIVE FFR
Clinical Context and Test Purpose
The purpose of selective noninvasive FFR-CT in patients with stable chest pain who have suspected SIHD
and who are being considered for ICA is to select patients who may be managed safely with observation
only, instead of undergoing ICA in the short term.
The following PICOTS were used to select literature to inform this review.
Patients
The population of interest includes patients with stable chest pain at intermediate risk of CAD (i.e., with
suspected or presumed SIHD) who are being considered for ICA. Patients may have undergone prior
noninvasive testing and been treated for presumed stable angina.
Interventions
The intervention of interest is CCTA with selective FFR-CT when CCTA shows evidence of coronary artery
stenosis.
Comparators
The comparator of interest is CCTA may be performed alone without FFR-CT. Individuals may proceed
directly to ICA. Conventional noninvasive imaging tests providing functional information, including
myocardial perfusion imaging (MPI) using SPECT, stress echocardiography (SECHO), and cardiac PET,
may be used prior to ICA. Cardiovascular MRI is also an option.
Outcomes
The final outcomes of interest include ICA rates, ICA without obstructive CAD, major adverse
cardiovascular events (MACE), and adverse events attributed to testing and treatment.
The intermediate outcome of interest is the ability of the test to distinguish clinically significant CAD for
which revascularization may provide benefit.
Timing
Rates of ICA and treatment-related morbidity are typically short-term (e.g., ≤3 months). In addition, rates of
subsequent ICA, treatment-related morbidity, MACE, quality of life
(QOL), and resource utilization
ascertained over a period of 1 to 3 years are also of interest.
©2017 Blue Cross and Blue Shield of Louisiana
Blue Cross and Blue Shield of Louisiana is an independent licensee of the Blue Cross and Blue Shield Association and incorporated
as Louisiana Health Service & Indemnity Company.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic,
mechanical, photocopying, or otherwise, without permission from Blue Cross and Blue Shield of Louisiana.
Page 5 of 21

Coronary Computed Tomography Angiography With Selective Noninvasive Fractional Flow Reserve
Policy #
00537
Original Effective Date:
02/15/2017
Current Effective Date:
10/18/2017
Setting
The setting is a general cardiology practice for patients undergoing nonemergent chest pain evaluation.
Technical Performance
Data supporting technical performance derive from the test-retest reliability of FFR-CT and invasively
measured FFR (reference standard). Other technical performance considerations were summarized in the
FDA documentation.
Johnson et al (2015) reported on the repeatability of invasive FFR. Data from 190 paired assessments were
analyzed (patients measured twice over
2 minutes). The test-retest coefficient of variation of
2.5%
(r2=98.2%) was reported using a “smart minimum” in the analyses (“the lowest average of 5 consecutive
cardiac cycles of sufficient quality within a run of 9 consecutive quality beats”). Hulten and Di Carli (2015)
noted that based on the Johnson results, an FFR of 0.8 would have a 95% confidence interval (CI) of 0.76
to 0.84. Gaur et al (2014) analyzed data from 28 patients (58 vessels) with repeated FFR-CT and invasive
FFR measurements. They reported coefficients of variation of 3.4% (95% CI, 1.5% to 4.6%) for FFR-CT
and 2.7% (95% CI, 1.8% to 3.3%) for invasive FFR. Although reproducibility was acceptable, whether test-
retest reliability over time might be similar is unclear.
The ability to obtain FFR-CT measurements is directly related to the quality of imaging data and values are
not calculated for small vessels (<1.8 mm). Nitrate administration is recommended (generally standard
practice unless contraindicated) for vasodilatation, and a lack of nitrates can affect FFR-CT results. In
addition, the FDA de novo summary lists factors that can adversely impact FFR-CT results, including:
imaging data quality, incorrect brachial pressure, myocardial dysfunction and hypertrophy, and abnormal
physiology (e.g., congenital heart disease). Coronary calcium might also impact measurements.
Section Summary: Technical Performance
Reported results have indicated that the test-retest reliability is acceptable and other known factors can
impact variability of FFR-CT results.
Diagnostic Accuracy
Studies Included in FFR-CT Systematic Reviews: Per-Patient Diagnostic Accuracy
Twenty-six studies have contributed patient-level results to a 2015 meta-analysis that examined 5 non-FFR-
CT imaging modalities (see Table 1). Five studies contributed results to 2 meta-analyses, Wu et al (2016)
and Danad et al (2017), evaluating the diagnostic accuracy of FFR-CT using patients as the unit of analysis.
Only the FDA-cleared HeartFlow software has been evaluated prospectively across multiple sites. Two
small retrospective studies have reported per-patient performance characteristics for the prototype Siemens
workstation-based software. The 3 HeartFlow FFRCT studies used successive software versions with
reported improvement in specificity (from 54% to 79%) between versions 1.2 and 1.4. The NXT Trial, the
basis for device clearance by FDA, was conducted at 11 sites in 8 countries (Canada, EU, Asia). Although
not examined in the 2 included meta-analyses, subgroup analyses suggested little variation in results by
sex and age. Effectively, the entirety of the data was obtained in patients of white or Asian decent; almost
all patients were appropriate for testing according to FDA clearance.
©2017 Blue Cross and Blue Shield of Louisiana
Blue Cross and Blue Shield of Louisiana is an independent licensee of the Blue Cross and Blue Shield Association and incorporated
as Louisiana Health Service & Indemnity Company.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic,
mechanical, photocopying, or otherwise, without permission from Blue Cross and Blue Shield of Louisiana.
Page 6 of 21

Coronary Computed Tomography Angiography With Selective Noninvasive Fractional Flow Reserve
Policy #
00537
Original Effective Date:
02/15/2017
Current Effective Date:
10/18/2017
Danad et al
Danad et al (2017) included 23 studies published between January 2002 and February 2015 evaluating the
diagnostic performance of CCTA, FFR-CT, SPECT, SECHO, MRI, or ICA compared with an invasive FFR
reference standard. The 3 included FFR-CT studies used the HeartFlow software and had performed FFR
in at least 75% of patients. A cutoff of 0.75 defined significant stenosis in 8 (32%) studies and in the
remainder 0.80 (the current standard used in all FFR-CT studies). Per-patient and per-vessel meta-
analyses were performed. Study quality was assessed using QUADAS-2; no significant biases were
identified in FFR-CT studies but a high risk of biased patient selection was judged in 10 (43.4%) of other
studies. HeartFlow funded publication Open Access; 1 author was a consultant to, and another a cofounder
of, HeartFlow.
On the patient level, MRI had the highest combined sensitivity (90%; 95% CI, 75% to 97%) and specificity
(94%; 95% CI, 79% to 99%) for invasive FFR, but were estimated from only 2 studies (70 patients). FFR-CT
had similar sensitivity (90%; 95% CI, 85% to 93%), but lower specificity (71%; 95% CI, 65% to 75%), and
accordingly a lower positive likelihood ratio (3.34; 95% CI, 1.78 to 6.25) than MRI (10.31; 95% CI, 3.14 to
33.9). The negative likelihood ratios were low (lower is better) for both FFR-CT (0.16; 95% CI, 0.11 to 0.23)
and MRI (0.12; 95% CI, 0.05 to 0.30); however, the CI is more narrow for FFR-CT due to larger sample for
FFR-CT. CCTA had a slightly higher negative likelihood ratio (0.22; 95% CI, 0.10 to 0.50). Results for the
per-vessel area under the summary receiver operating characteristic curve were similar except for CCTA
where per-patient results were considerably worse (e.g., C statistic of 0.57 vs. 0.85). Reviewers noted
heterogeneity in many estimates (e.g., CCTA sensitivity, I2=80%). Finally, pooled results for some imaging
tests included few studies.
Wu et al
Wu et al (2016) identified 7 studies (833 patients, 1377 vessels) comparing FFR-CT with invasively
measured FFR from searches of PubMed, Cochrane, EMBASE, Medion, and meeting abstracts through
January 2016. Studies included patients with established or suspected SIHD. In addition to the 3 FFR-CT
studies pooled by Danad et al, 1 additional study using HeartFlow technique (44 patients; 48 vessels) and 3
additional studies (180 patients; 279 vessels) using Siemens cFFR software (not FDA approved or cleared)
were identified. An invasive FFR cutoff of 0.80 was the reference standard in all studies. Per-patient results
reported in 5 studies were pooled and reported in Table 1. All studies were rated at low risk of bias and
without applicability concerns using the QUADAS-2 tool. Appropriate bivariate meta-analyses (accounting
for correlated sensitivity and specificity) were used.
As expected given study overlap, FFR-CT performance characteristics were similar to those reported by
Danad et al, but with a slightly higher specificity (see Table 1). The pooled per-vessel C statistic was lower
(0.86) than the per-patient result (0.90). No evidence of publication bias was detected, but the number of
studies was too small to adequately assess. Reviewers noted that, in 2 studies, FFR-CT results were
uninterpretable in 12.0% and 8.2% of participants.
©2017 Blue Cross and Blue Shield of Louisiana
Blue Cross and Blue Shield of Louisiana is an independent licensee of the Blue Cross and Blue Shield Association and incorporated
as Louisiana Health Service & Indemnity Company.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic,
mechanical, photocopying, or otherwise, without permission from Blue Cross and Blue Shield of Louisiana.
Page 7 of 21
Coronary Computed Tomography Angiography With Selective Noninvasive Fractional Flow Reserve
Policy #
00537
Original Effective Date:
02/15/2017
Current Effective Date:
10/18/2017
Takx et al
Takx et al (2015) identified studies reporting on the ability of perfusion CT, MRI, SECHO, PET, and SPECT
to detect hemodynamically significant CAD as measured by ICA with invasive FFR. Studies published
through May 2014 were eligible for inclusion; PubMed, EMBASE, and Web of Science were searched.
QUADAS-2 was used to assess study quality; studies generally rated poorly on blinding of the index test
result from the assessor and study population selection. Reviewers designated the negative likelihood ratio
as the diagnostic characteristic of interest (i.e., ability to exclude disease) noting that MPI (e.g., MRI,
SPECT, PET, or CT) has been proposed to be a gatekeeper to ICA. No funding was obtained for the review
and the study was registered on PROSPERO (the 2 other meta-analyses were not).
The pooled negative likelihood ratios for MRI, PET, and perfusion CT were similar in magnitude (0.12 to
0.14; see Table 1) although the CI for PET was wide. Heterogeneity among studies included in the pooled
patient-level results was considered high for PET
(I2=84%), moderate for CT (I2=70%) and SPECT
(I2=55%), and low for MRI (I2=0%) and SECHO (I2=0%). Publication bias, when able to be assessed, was
not suspected. With respect to ability to detect hemodynamically significant ischemia, reviewers concluded
that “MPI with MRI, CT, or PET has the potential to serve as a gatekeeper for invasive assessment of
hemodynamic significance by ICA and FFR.” Studies of FFR-CT were not included in the analysis.
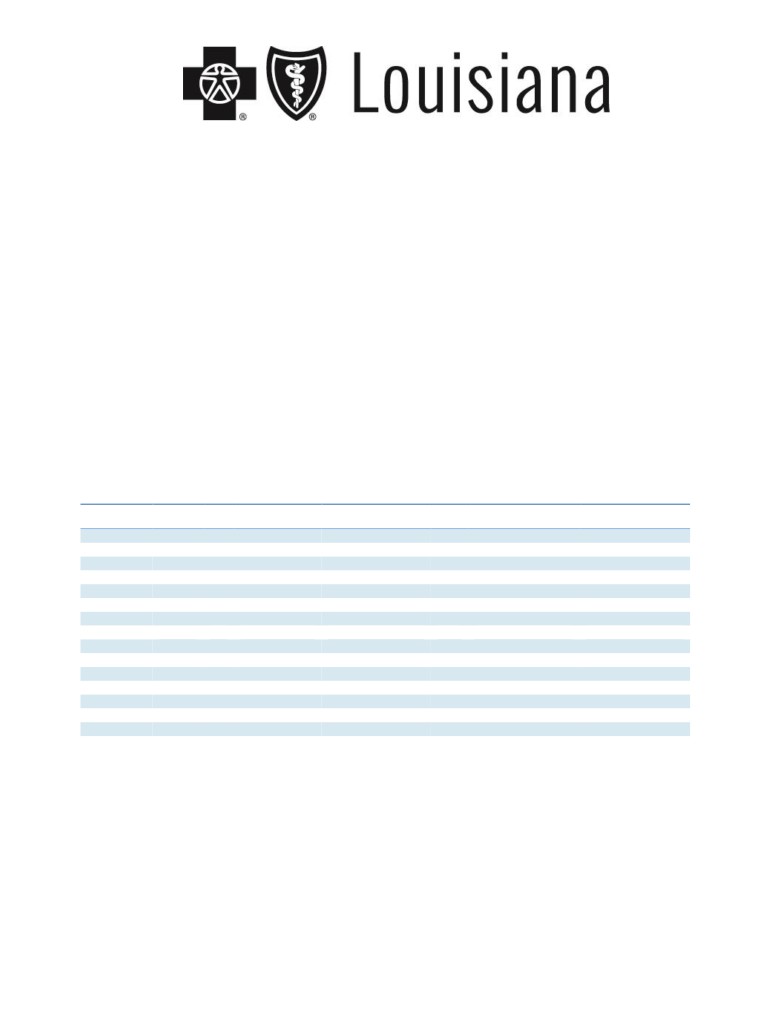
Table 1. Pooled Per-Patient Pooled Diagnostic Performance of Noninvasive Tests for Invasive FFR
Sensitivity
Specificity
Test
Studies
N
(95% CI)
(95% CI)
C
LR+ (95% CI)
LR- (95% CI)
Danad et al (2017)
MRI
2
70
90% (75 to 97)
94% (79 to 99)
0.94
10.3 (3.14 to 33.9)
0.12 (0.05 to 0.30)
FFR-CT
3
609
90% (85 to 93)
71% (65 to 75)
0.94
3.3 (1.78 to 6.25)
0.16 (0.11 to 0.23)
CCTA
4
694
90% (86 to 93)
39% (34 to 44)
0.57
1.5 (1.25 to 1.90)
0.22 (0.10 to 0.50)
SECHO
2
115
77% (61 to 88)
75% (63 to 85)
0.82
3.0 (1.94 to 4.65)
0.34 (0.17 to 0.66)
SPECT
3
110
70% (59 to 80)
78% (68 to 87)
0.79
3.4 (1.04 to 11.1)
0.40 (0.19 to 0.83)
ICA
2
954
69% (65 to 75)
67% (63 to 71)
0.75
2.5 (1.25 to 5.13)
0.46 (0.39 to 0.55)
Wu et al (2016)
FFR-CT
5
833
89% (85 to 93)
76% (64 to 84)
0.90
3.7 (2.41 to 5.61)
0.14 (0.09 to 0.21)
Takx et al (2015)
MRI
10
798
89% (86 to 92)
87% (83 to 90)
0.94
6.3 (4.88 to 8.12)
0.14 (0.10 to 0.18)
PCT
5
316
88% (82 to 92)
80% (73 to 86)
0.93
3.8 (1.94 to 7.40)
0.12 (0.04 to 0.33)
SECHO
4
177
69% (56 to 79)
84% (75 to 90)
0.83
3.7 (1.89 to 7.15)
0.42 (0.30 to 0.59)
SPECT
8
533
74% (67 to 79)
79% (74 to 83)
0.82
3.1 (2.09 to 4.70)
0.39 (0.27 to 0.55)
PET
2
224
84% (75 to 91)
87% (80 to 92)
0.93
6.5 (2.83 to 15.1)
0.14 (0.02 to 0.87)
CCTA: coronary computed tomography angiography; CI: confidence interval; FFR-CT: fractional flow reserve using coronary computed
tomography angiography; ICA: invasive coronary angiography; LR: likelihood ratio; MRI: magnetic resonance imaging; PCT: perfusion
computed tomography; PET: positron emission tomography; SECHO: stress echocardiography; SPECT: single-photon emission
computed tomography.
Section Summary: Diagnostic Accuracy
Three studies including 609 patients have evaluated diagnostic accuracy of the FDA-cleared HeartFlow
software. Software used in successive studies was also revised to improve performance characteristics,
©2017 Blue Cross and Blue Shield of Louisiana
Blue Cross and Blue Shield of Louisiana is an independent licensee of the Blue Cross and Blue Shield Association and incorporated
as Louisiana Health Service & Indemnity Company.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic,
mechanical, photocopying, or otherwise, without permission from Blue Cross and Blue Shield of Louisiana.
Page 8 of 21
Coronary Computed Tomography Angiography With Selective Noninvasive Fractional Flow Reserve
Policy #
00537
Original Effective Date:
02/15/2017
Current Effective Date:
10/18/2017
particularly specificity. For example, using an earlier software version, the DeFACTO Trial reported a
specificity of
54%. Accordingly, pooled results from the Danad systematic review must be interpreted
carefully. In addition, there is some uncertainty in the generalizability of results obtained in these studies
conducted under likely controlled conditions (e.g., data from the NXT Trial forming the basis for FDA
clearance).
Given the purpose to avoid ICA, the negative likelihood ratio, or how a negative result might dissuade a
clinician from proceeding to ICA, is of primary interest—i.e., excluding a patient with vessels having a high
FFR from ICA. While CIs are relatively wide and overlapping, the negative likelihood ratio estimates of FFR-
CT for excluding physiologically significant coronary stenoses tended to be lower (i.e., better) than CCTA
alone, SECHO, SPECT, and ICA. Only MRI yielded a similarly low or lower negative likelihood ratio than
FFR-CT.
Clinical Utility
Indirect Evidence
Diagnostic performance can offer indirect evidence of clinical utility, assuming providers act according to a
test result. As previously noted, an effective gatekeeper strategy must be able to decrease the probability of
disease (rule out) sufficiently that a planned ICA would not be performed. Ruling out disease is a function of
the negative likelihood ratio that defines the degree to which a negative test decreases the posttest odds
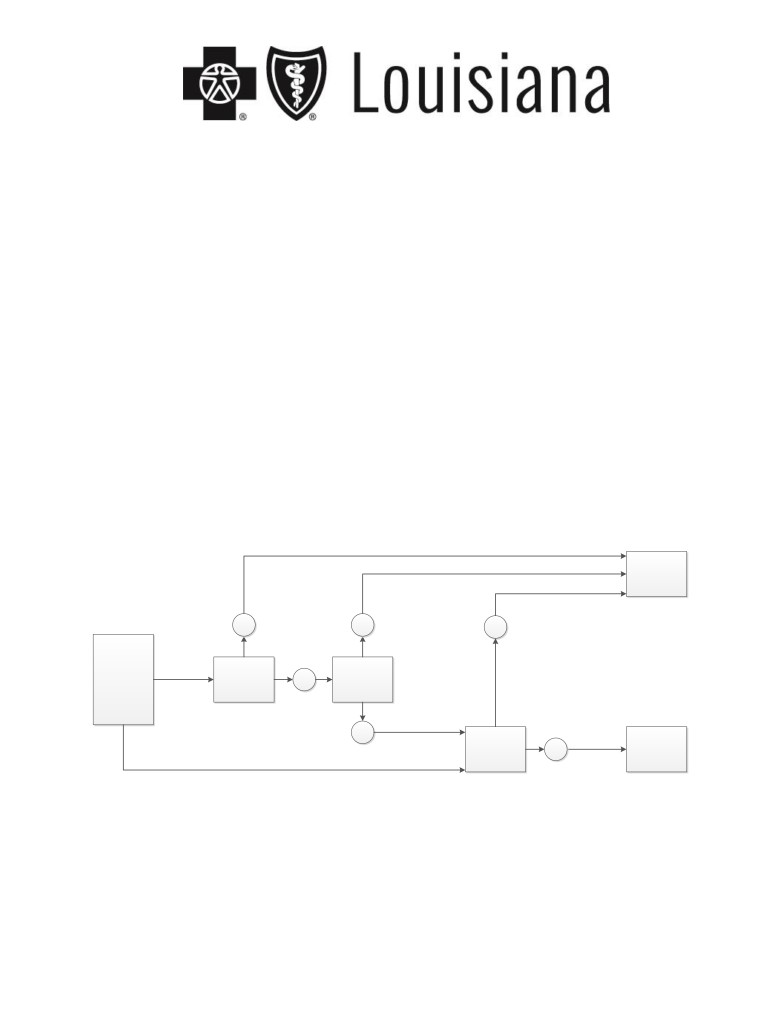
(and probability) of disease. The steps in the logic are illustrated in Figure 1.
Figure 1. Pathway for Clinical Use of FFR-CT to Support Clinical Utility
Optimal Medical
Therapy
Low Negative
Likelihood Ratio
identifies additional
individuals with low
disease probability
-
-
who may avoid
-
Invasive Coronary
Stable Chest Pain
Angiography
with Intermediate
Risk of Coronary
Artery Disease Being
Coronary Computed
Considered for
Tomography
+
Add FFR-CT
Invasive Coronary
Angiography
Angiography
(CCTA)
(ie, Suspected Stable
Ischemic Heart
Disease)
+
Invasive Coronary
Obstructive
Angiography
Coronary Artery
(with invasive FFR if
+
Disease and
needed)
Revascularization
FFR-CT: fractional flow reserve using coronary computed tomography angiography.
Table 2 illustrates how a negative test would lower the probability of a hemodynamically significant
obstruction from pretest probabilities of 0.25, 0.50, or 0.75 for the various tests examined in the meta-
©2017 Blue Cross and Blue Shield of Louisiana
Blue Cross and Blue Shield of Louisiana is an independent licensee of the Blue Cross and Blue Shield Association and incorporated
as Louisiana Health Service & Indemnity Company.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic,
mechanical, photocopying, or otherwise, without permission from Blue Cross and Blue Shield of Louisiana.
Page 9 of 21
Coronary Computed Tomography Angiography With Selective Noninvasive Fractional Flow Reserve
Policy #
00537
Original Effective Date:
02/15/2017
Current Effective Date:
10/18/2017
analyses. For example, according to the results of Danad et al, if the pretest probability was 0.50, following
a negative CCTA study the posttest probability would be 0.18 (95% CI, 0.09 to 0.33); and following a
negative SECHO, 0.25 (95% CI, 0.15 to 0.40) or SPECT, 0.29 (95% CI, 0.16 to 0.45). In contrast, beginning
with a pretest probability of 0.50, a negative FFR-CT would yield a posttest probability of 0.14 (95% CI, 0.10
to 0.19) (Danad et al) and 0.12 (95% CI, 0.08 to 0.17) (Wu et al). Overall, the negative likelihood ratios and
posttest probability estimates for FFR-CT are slightly better than CCTA as well as SECHO and SPECT.
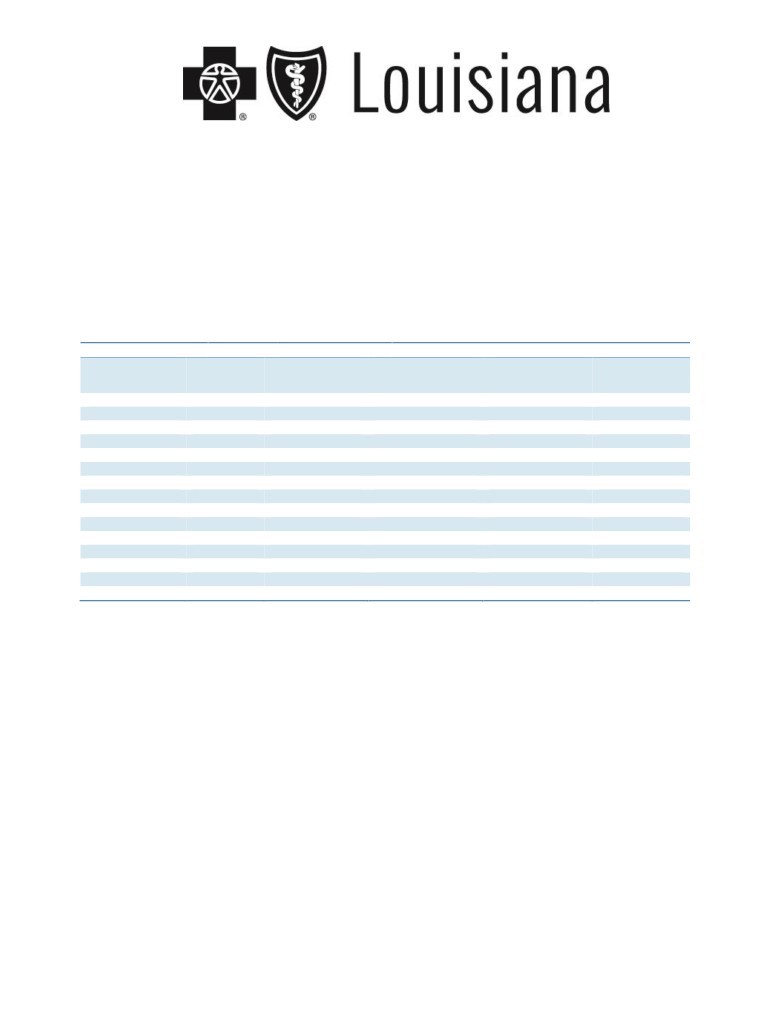
Table 2. Change in Disease Probability Following a Negative Test
Posttest Probability (95% CI) After Negative Test
Study
Modality
Negative LR
Pretest Probability
Pretest Probability
Pretest
(95% CI)
0.25
0.50
Probability
0.75
Danad et al (2016)
MRI
0.12 (0.05 to 0.30)
0.04 (0.02 to 0.09)
0.11 (0.05 to 0.23)
0.26 (0.13 to 0.47)
FFR-CT
0.16 (0.11 to 0.23)
0.05 (0.04 to 0.07)
0.14 (0.10 to 0.19)
0.32 (0.25 to 0.41)
CCTA
0.22 (0.10 to 0.50)
0.07 (0.03 to 0.14)
0.18 (0.09 to 0.33)
0.40 (0.23 to 0.60)
SECHO
0.34 (0.17 to 0.66)
0.10 (0.05 to 0.18)
0.25 (0.15 to 0.40)
0.50 (0.34 to 0.66)
SPECT
0.40 (0.19 to 0.83)
0.12 (0.06 to 0.22)
0.29 (0.16 to 0.45)
0.55 (0.36 to 0.71)
ICA
0.46 (0.39 to 0.55)
0.13 (0.12 to 0.15)
0.32 (0.28 to 0.35)
0.58 (0.54 to 0.62)
Wu et al (2016)
FFR-CT
0.14 (0.09 to 0.21)
0.04 (0.03 to 0.07)
0.12 (0.08 to 0.17)
0.30 (0.21 to 0.39)
Takx et al (2015)
MRI
0.14 (0.10 to 0.18)
0.04 (0.03 to 0.06)
0.12 (0.09 to 0.15)
0.30 (0.23 to 0.35)
Perfusion CT
0.12 (0.04 to 0.33)
0.04 (0.01 to 0.10)
0.11 (0.04 to 0.25)
0.26 (0.11 to 0.50)
SECHO
0.42 (0.30 to 0.59)
0.12 (0.09 to 0.16)
0.30 (0.23 to 0.37)
0.56 (0.47 to 0.64)
SPECT
0.39 (0.27 to 0.55)
0.12 (0.08 to 0.15)
0.28 (0.21 to 0.35)
0.54 (0.45 to 0.62)
PET
0.14 (0.02 to 0.87)
0.04 (0.01 to 0.22)
0.12 (0.02 to 0.47)
0.30 (0.06 to 0.72)
CCTA: coronary computed tomography angiography; CI: confidence interval; CT: computed tomography; FFR-CT: fractional flow
reserve using coronary computed tomography angiography; ICA: invasive coronary angiography; LR: likelihood ratio; MRI: magnetic
resonance imaging; PET: positron emission tomography; SECHO: stress echocardiography; SPECT: single-photon emission
computed tomography.
We identified 1 study (Curzen et al, 2016) that examined 200 consecutive individuals selected from the NXT
trial population “to reproduce the methodology of the invasive RIPCORD study” with elective management
of stable chest pain. All subjects received CCTA including FFR-CT “in at least 1 vessel with diameter ≥ 2
mm and diameter stenosis ≥ 30%” as well as ICA within 60 days of CCTA. Three experienced interventional
cardiologists reviewed the CCTA results (initially without the FFR-CT results) and selected a management
plan from the following 4 options: “1) OMT alone; 2) PCI + OMT; 3) coronary artery bypass graft + OMT; or
4) more information about ischemia required - they committed to option 1 by consensus.” Following the
initial decision, results from the FFR-CT were shared with the same group of interventional cardiologists
who again made a decision by consensus based on the same 4 options. A cutoff of 0.80 or less was
considered significant on FFR-CT. A stenosis was considered significant on CCTA or ICA with 50% or more
diameter narrowing. Change in management between the first decision based on CCTA only and the
second decision based on CCTA plus FFR-CT was the primary end point of this study. Secondary end
©2017 Blue Cross and Blue Shield of Louisiana
Blue Cross and Blue Shield of Louisiana is an independent licensee of the Blue Cross and Blue Shield Association and incorporated
as Louisiana Health Service & Indemnity Company.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic,
mechanical, photocopying, or otherwise, without permission from Blue Cross and Blue Shield of Louisiana.
Page 10 of 21

Coronary Computed Tomography Angiography With Selective Noninvasive Fractional Flow Reserve
Policy #
00537
Original Effective Date:
02/15/2017
Current Effective Date:
10/18/2017
points included analysis of the vessels considered to have significant stenosis based on CCTA alone versus
CCTA plus FFR-CT as well as vessels identified as targets for revascularization based on CCTA alone
versus CCTA plus FFR-CT. This study was conducted by investigators in the United Kingdom and
Denmark. Funding was provided by HeartFlow and multiple authors reported receiving fees, grants, and/or
support from HeartFlow.
Results for the primary end point (see Table 3) yielded a change in management category for 72 of 200
(36%) individuals. For the 87 individuals initially assigned to PCI based on CCTA alone, the addition of the
FFR-CT results shifted management for 26 of 87 (30%) to OMT (i.e., no ischemic lesion on FFR-CT) and an
additional 16 (18%) individuals remained in the PCI category but FFR-CT identified a different target vessel
for PCI. These findings provide supportive information that the improved diagnostic accuracy of FFR-CT in
particular related to its better negative likelihood ratio compared to CCTA alone would likely lead to changes
in management that would be expected to improve health outcomes.
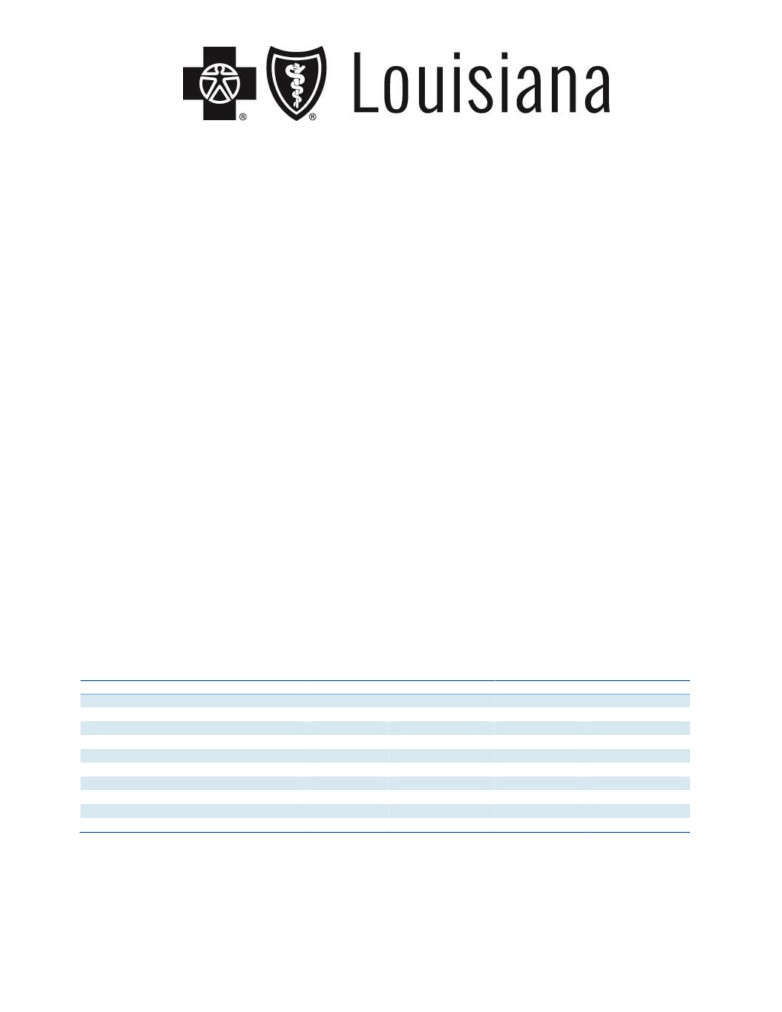
Table 3. Summary of Overall Changes to Management in Patients Using CCTA vs CCTA + FFR-CT
Management Category Consensus
CCTA Alone,
CCTA + FFR-CT,
Strategy Changea
Decision
n (%)
n (%)
(95% CI)
More data required
38 (19.0%)
0
Optimal medical therapy
67 (33.5%)
113 (56.5%)
23% (18% to 29%)
Percutaneous coronary intervention
87 (43.5%)
78 (39.0%)
-5% (-2% to -8%)
Coronary artery bypass graft surgery
8 (4.0%)
9 (4.5%)
0.5% (0.1% to 3%)
CCTA: coronary computed tomography angiography; CI: confidence interval; FFR-CT: fractional flow reserve using
coronary computed tomography angiography.
a
p<0.001 for between-group change, CCTA alone vs CCTA + FFR-CT.
Direct Evidence
We identified
2 prospective comparative studies including
1 prospective nonrandomized study that
compared an FFR-CT strategy (CCTA with noninvasive FFR measurement when requested or indicated)
with ICA and 1 randomized controlled trial that examined CCTA as a gatekeeper to ICA (see Tables 4 and
5). In addition, we identified 1 prospective cohort study and 2 retrospective cohort studies of patients
referred for CCTA, which included FFR-CT evaluation.
PLATFORM Study
The Prospective LongitudinAl Trial of FFRCT: Outcome and Resource Impacts
(PLATFORM) study
compared diagnostic strategies with or without FFR-CT in patients with suspected stable angina but without
known CAD. The study was conducted at 11 EU sites. All testing was nonemergent. Patients were divided
into 2 strata, according to whether the test planned prior to study enrollment was: (1) noninvasive or (2) ICA
(the patient population of interest in this evidence review). Patients were enrolled in consecutive cohorts,
with the first cohort undergoing a usual care strategy followed by a second cohort provided CCTA with FFR-
CT performed when requested (recommended if stenoses ≥30% were identified). Follow-up was scheduled
at 90 days and 6 and 12 months after entry (99.5% of patients had 1-year follow-up data). Funding was
©2017 Blue Cross and Blue Shield of Louisiana
Blue Cross and Blue Shield of Louisiana is an independent licensee of the Blue Cross and Blue Shield Association and incorporated
as Louisiana Health Service & Indemnity Company.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic,
mechanical, photocopying, or otherwise, without permission from Blue Cross and Blue Shield of Louisiana.
Page 11 of 21

Coronary Computed Tomography Angiography With Selective Noninvasive Fractional Flow Reserve
Policy #
00537
Original Effective Date:
02/15/2017
Current Effective Date:
10/18/2017
provided by HeartFlow and multiple authors reported receiving fees, grants, and/or support from HeartFlow.
Data analyses were performed by the Duke Clinical Research Institute.
ICA without obstructive disease at 90 days was the primary end point in patients with planned invasive
testing—“no stenosis ≥ 50% by core laboratory quantitative analysis or invasive FFR < 0.80.” Secondary
end points included ICA without obstructive disease following planned noninvasive testing, and (1) MACE at
1 year defined as a composite of all-cause mortality, MI, and urgent revascularization and (2) MACE and
vascular events within 14 days. QOL was evaluated using the Seattle Angina Questionnaire, and EQ-5D (5-
item and 100-point visual analog scale). CCTA studies were interpreted by site investigators; quantitative
coronary angiography measurements were performed at a central laboratory, as was FFR-CT. Cumulative
radiation was also assessed. A sample size of 380 patients in the invasive strata yielded a 90% power to
detect a 50% decrease in the primary end point given a 30% event rate (ICA without obstructive disease)
with a usual care strategy and a dropout rate up to 10%.
ICA was planned in 380 participants, of whom 193 (50.8%) had undergone prior noninvasive testing. The
mean pretest probability in the planned ICA strata was approximately 50% (51.7% and 49.4% in the 2
groups). FFR-CT was requested in 134 patients and successfully obtained in 117 of 134 (87.3%) in the
FFR-CT group. At 90 days, 73.3% of those in the usual care group had no obstructive findings on ICA
compared with 12.4% in the FFR-CT group based on core laboratory readings (56.7% and 9.3% based on
site readings). The difference was similar in a propensity-matched analysis of a subset of participants
(n=148 from each group or 78% of the entire sample). Prior noninvasive testing did not appear associated
with nonobstructive findings. MACE rates were low and did not differ between strategies. Mean level of
radiation exposure though 1 year was also similar in the usual care group (10.4 mSv) and the planned ICA
group (10.7 mSv). No differences in QOL were found between groups.
Results of the PLATFORM study support the notion that, in patients with planned ICA, FFR-CT can
decrease the rate of ICAs and unnecessary procedures (finding no significant obstructive disease) and that
FFR-CT may provide clinically useful information to physicians and patients. Study limitations include a
nonrandomized design; high rate of no obstructive disease with a usual care strategy (73.3%), which was
higher than the 30% rate assumed in the sample size estimates; and a sample size that was small with
respect to evaluating adverse cardiac events. Although finding a large effect in patients with planned
invasive testing, the nonrandomized design limits causal inferences and certainty that the magnitude of
effect. The propensity-matched analysis (in a matched subset) offers some reassurance, but the sample
size was likely too small to provide robust results.
CAD-Man Trial
Dewey et al (2016) conducted the Coronary Artery Disease Management (CAD-Man) trial, a single-center,
parallel-group assignment trial examining CCTA as a gatekeeper to ICA in patients with atypical angina or
chest pain and suspected CAD who were indicated for ICA. Patients were randomized to direct ICA or to
ICA only if a prior CCTA was positive (a stenosis ≥70% stenosis in any vessel or ≥50% in the left main
coronary artery). The trialists reported that when obstructive disease was suspect following CCTA, late
enhancement MRI was performed to evaluate the extent of viable myocardium (completed in 17 patients) to
©2017 Blue Cross and Blue Shield of Louisiana
Blue Cross and Blue Shield of Louisiana is an independent licensee of the Blue Cross and Blue Shield Association and incorporated
as Louisiana Health Service & Indemnity Company.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic,
mechanical, photocopying, or otherwise, without permission from Blue Cross and Blue Shield of Louisiana.
Page 12 of 21
Coronary Computed Tomography Angiography With Selective Noninvasive Fractional Flow Reserve
Policy #
00537
Original Effective Date:
02/15/2017
Current Effective Date:
10/18/2017
guide revascularization; however, the study protocol clarified that MRI was not used for decisions to
proceed to ICA. A major procedural complication
(death, stroke, MI, or event requiring
>24-hour
hospitalization) within
24 hours was the primary outcome; secondary outcomes included ICA with
obstructive CAD (diagnostic yield), revascularizations, and MACE during long-term follow-up. The trial was
performed in Germany. Patients were excluded if they had evidence of ischemia or signs of MI and just over
half (56.5%) were inpatients at the time of enrollment. Obstructive disease was defined as “at least one
50% diameter stenosis in the left main coronary artery or at least one 70% diameter stenosis in other
coronary arteries.” Allocation concealment appeared adequate, but the trial was unblinded owing to the
nature of the intervention. In addition, the mean pretest probability of CAD at baseline was higher in the
ICA-only arm (37.3% vs. 31.3%; see Table 4). The research was supported by public funding.
ICAs were reduced by 85.6% in the CCTA arm and by 80.9% for ICA with no obstructive disease. A major
procedural complication (the primary outcome) occurred in a single patient undergoing CCTA. PCIs were
less frequent when CCTA was performed—9.6% versus 14.2% (p<0.001). Over a median follow-up of 3.3
years, MACE rates were similar in the trial arms (4.2% in the CCTA group vs 3.7% with ICA; adjusted
hazard ratio [HR], 0.90; 95% CI, 0.30 to 2.69). In the CCTA arm, there was 1 death, 2 patients with unstable
angina, and 6 revascularizations; in the ICA arm there was 1 MI, 1 stroke, and 5 revascularizations.
The trial demonstrated that CCTA as a gatekeeper to planned ICA can avoid a large number of procedures, a
corresponding increase in the diagnostic yield, and fewer revascularizations. Of note, the prevalence of
obstructive CAD found on ICA in this study population was 13% (43/334 eligible for primary outcome
analysis), which is lower than the prevalence of obstructive CAD in the PLATFORM population (26.7%).
Thus, the subset of individuals who went onto ICA following CCTA findings of obstructive CAD was 20
(12%) of 167 eligible for primary outcome analysis and only 3 (1.7%) were found to have no obstructive
CAD on ICA. MACE rates did not differ between arms. The trial was powered neither to detect a difference
nor to assess noninferiority—implications of the absence of a difference are limited. Finally, although the
patient population included those scheduled for elective ICA, it was heterogeneous, including those with
recent onset and longer standing chest pain. The single-center nature of the trial is an additional limitation;
a subsequent multicenter trial (DISCHARGE) is ongoing.
Table 4. Characteristics of Comparative Studies
Characteristics
Nonrandomized
Randomized
PLATFORM
CAD-Man
ICA
FFR-CT
ICA
CCTA
(n=187)
(n=193)
(n=162)
(n=167)
Age (SD), y
63.4
(10.9)
60.7
(10.2)
60.4
(11.4)
60.4
(11.3)
Female, n (%)
79 (42.2%)
74 (38.3%)
88 (52.7%)
78 (48.1%)
Race/ethnic minority, n (%)
2 (1.1%)
1 (0.5%)
Pretest probability obstructive CAD, %
51.7%
49.4%
(17.2%)
37.3%
(24.8%)
31.3%
(21.1%)
Angina (%)
Typical
52 (27.8%)
45 (23.3%)
Atypical
122 (65.2%)
142 (73.6%)
79 (48.8%)
65 (38.9%)
©2017 Blue Cross and Blue Shield of Louisiana
Blue Cross and Blue Shield of Louisiana is an independent licensee of the Blue Cross and Blue Shield Association and incorporated
as Louisiana Health Service & Indemnity Company.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic,
mechanical, photocopying, or otherwise, without permission from Blue Cross and Blue Shield of Louisiana.
Page 13 of 21
Coronary Computed Tomography Angiography With Selective Noninvasive Fractional Flow Reserve
Policy #
00537
Original Effective Date:
02/15/2017
Current Effective Date:
10/18/2017
Noncardiac
12 (7.0%)
5 (2.6%)
80 (49.4%)
97 (58.1%)
Other chest discomfort
3 (1.8%)
5 (3.0%)
Prior noninvasive testing, n (%)
92 (49.2%)
101 (52.3%)
84 (50.3%)
92 (56.8%)
Diabetes, n (%)
36 (19.3%)
30 (15.5%)
30 (18.5%)
15 (9.0%)
Current smoker
34 (21.0%)
41 (24.5%)
Current or past smoker
103 (55.1%)
101 (52.3%)
85 (52.4%)
88 (52.6%)
CAD: coronary artery disease; CCTA: coronary computed tomography angiography; FFR-CT: fractional flow
reserve using coronary computed tomography angiography; ICA: invasive coronary angiography.
Table 5. Results of Comparative Studies
Outcomes
Nonrandomized
Randomized
PLATFORM
CAD-Man
ICA
FFR-CT
ICA
CCTA
(n=187)
(n=193)
(n=162)
(n=167)
Noninvasive FFR-CT
Requested, n (%)
134 (69.4%)
Successfully performed, n (%)
117 (60.1%)
ICA no obstructive disease, n (%)
137 (73.3%)
24 (12.4%)
137 (84.5%)
6 (3.6%)
Absolute difference (95% CI), %
60.8% (53.0% to 68.7%)
80.9% (74.6% to 87.2%)
ICA, n (%)
187 (100%)
76 (39.4%)
162 (100%)
24 (14.4%)
Absolute difference (95% CI), %
60.6% (53.7% to 67.5%)
85.6% (80.3% to 90.9%)
Revascularization, n (%)
PCI
49 (26.2%)
55 (28.5%)
CABG
18 (9.6%)
10 (5.2%)
Any
67 (35.8%)
65 (33.7%)
23 (14.2%)
16 (9.6%)
1-year outcomes, n (%)
MACEa
2 (1.1%)
2 (1.0%)
MACEb
6 (3.7%)
7 (4.2%)
CABG: coronary artery bypass grafting; CI: confidence interval; FFR-CT: fractional flow reserve using coronary
computed tomography angiography; ICA: invasive coronary angiography; MACE: major adverse cardiovascular events;
PCI: percutaneous coronary intervention.
a
Death, myocardial infarction, unplanned urgent revascularization
b Cardiac death, myocardial infarction, stroke, unstable angina, any revascularization.
Møller Jensen et al Prospective Cohort
Møller Jensen et al (2017) reported on a single-institution study of 774 consecutive individuals with
suspicion of CAD referred for nonemergent ICA or CCTA. Subjects were analyzed in 2 groups: a low-
intermediate-risk group accounting for 76% of patients with mean pretest probability of CAD 31% and a
high-risk group accounting for 24% of patients with mean pretest probability of CAD 67%. Among the 745
who received CCTA, FFR-CT was selectively ordered in 28% of patients overall (23% in the low-
intermediate-risk group, 41% in the high-risk group). CCTA was considered inconclusive in 3% of subjects
and among those with conclusive CCTA, FFR-CT yielded few inconclusive results, with less than 3% of
cases. During a minimum 90-day follow-up, the combined testing strategy of selective FFR-CT following
CCTA resulted in avoiding ICA in 91% of low-intermediate-risk and 75% of high-risk individuals. None of the
©2017 Blue Cross and Blue Shield of Louisiana
Blue Cross and Blue Shield of Louisiana is an independent licensee of the Blue Cross and Blue Shield Association and incorporated
as Louisiana Health Service & Indemnity Company.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic,
mechanical, photocopying, or otherwise, without permission from Blue Cross and Blue Shield of Louisiana.
Page 14 of 21

Coronary Computed Tomography Angiography With Selective Noninvasive Fractional Flow Reserve
Policy #
00537
Original Effective Date:
02/15/2017
Current Effective Date:
10/18/2017
patients who avoided ICA based on CCTA with selective FFR-CT were associated with serious clinical
adverse events over an average of 157 days of follow-up.
Nørgaard et al Retrospective Cohort
Nørgaard et al (2017) reported on results from symptomatic patients referred for CCTA at a single center in
Denmark from May 2014 to April 2015. All data were obtained from medical records and registries; the
study was described as a “review” of diagnostic evaluations and apparently retrospectively conducted.
Follow-up through 6 to 18 months was ascertained. From 1248 referred patients, 1173 underwent CCTA;
858 received medical therapy,
82 underwent ICA, 44 MPI, and 189 FFR-CT (185 [98%] obtained
successfully). Of the 185 individuals who successfully obtained FFR-CT, FFR-CT demonstrated values of
0.80 or less in 1 or more vessels in 57 (31%) patients and 49 (86%) went on to ICA; whereas of the 128
with higher FFR-CT values, only 5 (4%) went on to ICA. Assuming ICA was planned for all patients
undergoing FFR-CT, these results are consistent with FFR-CT being able to decrease the rate of ICA.
However, implications are limited by the retrospective design, performance at a single center, and lack of a
comparator arm including one for CCTA alone.
Lu et al Retrospective Cohort
Lu et al (2017) retrospectively examined a subgroup referred to ICA from the completed PROspective
Multicenter Imaging Study for Evaluation of Chest Pain (PROMISE) trial. PROMISE was a pragmatic trial
comparing CCTA with functional testing for the initial evaluation of patients with suspected SIHD. Of 550
participants referred to ICA within 90 days, 279 were not considered for the analyses due to CCTA
performed without nitroglycerin
(n=139), CCTA not meeting slice thickness guidelines
(n=90), or
nondiagnostic studies (n=50). Of the remaining 271 patients, 90 scans were inadequate to obtain FFR-CT,
leaving 181 (33%) of those referred to ICA for analysis. Compared with those excluded, patients in the
analytic sample were less often obese, hypertensive, diabetic, minority, or reported a CAD equivalent
symptom. The 2 groups had similar pretest probabilities of disease, revascularization rates, and MACE, but
the distribution of stenoses in the analytic sample tended to be milder (p=0.06). FFR-CT studies were
performed in a blinded manner and not available during the conduct of PROMISE for decision making.
Severe stenoses (≥70%) or left main disease (≥50%) were present in 110 (66%) patients by CCTA result
and in 54% by ICA. Over a 29-month median follow-up, MACE (death, nonfatal MI, hospitalization for
unstable angina) or revascularization occurred in 51% of patients (9% MACE, 49% revascularization). A
majority (72%) of the sample had at least 1 vessel with an FFR-CT ≤0.80, which was also associated with a
higher risk of revascularization but with a wide CI (HR = 5.1; 95% CI, 2.6 to 11.5). If reserved for patients
with an FFR-CT of 0.80 or less, ICAs might have been avoided in 50 patients (i.e., reduced by 28%) and the
rate of ICA without 50% or more stenosis from 27% (calculated 95% CI, 21% to 34%) to 15% (calculated
95% CI, 10% to 23%). If the 90 patients whose images sent for FFR-CT but were unsatisfactory proceeded
to ICA—as would have occurred in practice—the rate of ICA might have decreased by 18% and ICA without
significant stenosis from 31% to 25%.
The authors suggested that when CCTA is used as the initial evaluation for patients with suspected SIHD,
adding FFR-CT could have decreased the referral rate to ICA in PROMISE from 12.2% to 9.5%, or close to
©2017 Blue Cross and Blue Shield of Louisiana
Blue Cross and Blue Shield of Louisiana is an independent licensee of the Blue Cross and Blue Shield Association and incorporated
as Louisiana Health Service & Indemnity Company.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic,
mechanical, photocopying, or otherwise, without permission from Blue Cross and Blue Shield of Louisiana.
Page 15 of 21

Coronary Computed Tomography Angiography With Selective Noninvasive Fractional Flow Reserve
Policy #
00537
Original Effective Date:
02/15/2017
Current Effective Date:
10/18/2017
the 8.1% rate observed in the PROMISE functional testing arm. They also noted similarity of their findings
to PLATFORM and concluded, “In this hypothesis-generating study of patients with stable chest pain
referred to ICA after [C]CTA, we found that adding FFRCT may improve the efficiency of referral to ICA,
addressing a major concern of an anatomic [C]CTA strategy. FFRCT has incremental value over anatomic
[C]CTA in predicting revascularization or MACE.”
This retrospective observational subgroup analysis from PROMISE suggests that when CCTA is the initial
noninvasive test for the evaluation of suspected SIHD, FFR-CT prior to ICA has the potential to reduce
unnecessary ICAs and increase the diagnostic yield. However, study limitations and potential
generalizability are important to consider. First, analyses included only a third of CCTA patients referred to
ICA and the some characteristics of the excluded group differed from the analytic sample. Second,
conclusions assume that an FFR-CT greater than
0.80 will always dissuade a physician from
recommending ICA and even in the presence of severe stenosis (e.g., ≥70% in any vessel or ≥50% in the
left main)—or almost half (46%) of patients with an FFR-CT greater than 0.80. Finally, estimates including
patients with either nondiagnostic CCTA studies (n=50) or studies inadequate for calculating FFR-CT
(n=90) are more appropriate because most likely those patients would proceed in practice to ICA.
Accordingly, the estimates are appropriately considered upper bounds for what might be seen in practice. It
is also important to note that in strata of the PLATFORM trial enrolling patients for initial noninvasive testing
(not planned ICA), ICA was more common following CCTA and contingent FFR-CT than following usual
care (18.3% vs. 12.0%) and ICA, with no obstructive disease more frequent in the FFR-CT arm (12.5% vs.
6.0%).
Section Summary: Clinical Utility
The evidence on the diagnostic performance characteristics, particularly showing higher specificity of FFR-
CT and better negative likelihood ratio as compared to CCTA alone, may be combined with indirect
evidence that CCTA with a selective FFR-CT strategy would likely lead to changes in management that
would be expected to improve health outcomes, particularly by limiting unnecessary ICA testing. Moreover,
there is direct evidence, provided by 2 prospective and 2 retrospective studies, that compares health
outcomes observed during 90-day to 1-year follow-up for strategies using CCTA particularly in combination
with selective FFR-CT with strategies using ICA or other noninvasive imaging tests. The available evidence
provides support that use of CCTA with selective FFR-CT is likely to reduce the use of ICA in individuals
with stable chest pain who are unlikely to benefit from revascularization by demonstrating the absence of
functionally significant obstructive CAD. In addition, the benefits are likely to outweigh potential harms given
that rates of revascularization for functionally significant obstructive CAD appear to be similar and cardiac-
related adverse events do not appear to be increased following a CCTA with selective FFR-CT strategy.
While individual studies are noted to have specific methodologic limitations and some variation is noted in
the magnitude of benefit across studies, in aggregate the evidence provides reasonable support that the
selective addition of FFR-CT following CCTA results in a meaningful improvement in the net health
outcome.
©2017 Blue Cross and Blue Shield of Louisiana
Blue Cross and Blue Shield of Louisiana is an independent licensee of the Blue Cross and Blue Shield Association and incorporated
as Louisiana Health Service & Indemnity Company.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic,
mechanical, photocopying, or otherwise, without permission from Blue Cross and Blue Shield of Louisiana.
Page 16 of 21

Coronary Computed Tomography Angiography With Selective Noninvasive Fractional Flow Reserve
Policy #
00537
Original Effective Date:
02/15/2017
Current Effective Date:
10/18/2017
SUMMARY OF EVIDENCE
For individuals with stable chest pain at intermediate risk of CAD; (i.e., suspected or presumed SIHD) being
considered for ICA who receive noninvasive FFR measurement following positive CCTA, the evidence
includes both direct and indirect evidence: 2 meta-analyses on diagnostic performance; 1 prospective,
multicenter nonrandomized comparative study; 1 prospective cohort; 2 retrospective cohort studies; and a
study reporting changes in management associated with CCTA-based strategies with selective addition of
FFR-CT and a randomized controlled trial (RCT) of CCTA alone compared with ICA. Relevant outcomes
are test accuracy and validity, morbid events, QOL, resource utilization, and treatment-related morbidity.
The meta-analyses indicated that CCTA has high sensitivity but moderately low specificity for
hemodynamically significant obstructive disease. Given the available evidence that CCTA alone has been
used to select patients to avoid ICA, the studies showing higher specificity of FFR-CT and lower negative
likelihood ratio of FFR-CT compared with CCTA alone, may be used to build a chain of evidence that CCTA
with a selective FFR-CT strategy would likely lead to changes in management that would be expected to
improve health outcomes by further limiting unnecessary ICA testing. Moreover, there is direct evidence,
provided by 2 prospective and 2 retrospective studies, that compares health outcomes observed during 90-
day to 1-year follow-up for strategies using CCTA particularly in combination with selective FFR-CT with
strategies using ICA or other noninvasive imaging tests. The available evidence provides support that use
of CCTA with selective FFR-CT is likely to reduce the use of ICA in individuals with stable chest pain who
are unlikely to benefit from revascularization by demonstrating the absence of functionally significant
obstructive CAD. In addition, the benefits are likely to outweigh potential harms because rates of
revascularization for functionally significant obstructive CAD appear to be similar and treatment-related
adverse events do not appear to increase following CCTA with a selective FFR-CT strategy. While
individual studies are noted to have specific methodologic limitations and some variation has been noted in
the magnitude of benefit across studies, in aggregate the evidence provides reasonable support that the
selective addition of FFR-CT following CCTA results in a meaningful improvement in the net health
outcome. The evidence is sufficient to determine that the technology results in meaningful improvements in
the net health outcome.
References
1.
Blue Cross and Blue Shield Association, Medical Policy Reference Manual, “Coronary Computed Tomography Angiography With
Selective Noninvasive Fractional Flow Reserve”, 6.01.59, 6:2017.
2.
Patel MR, Peterson ED, Dai D, et al. Low diagnostic yield of elective coronary angiography. N Engl J Med. Mar
11
2010;362(10):886-895. PMID 20220183
3.
Boden WE, O'Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med.
Apr 12 2007;356(15):1503-1516. PMID 17387127
4.
Fihn SD, Gardin JM, Abrams J, et al.
2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and
management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American
Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic
Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society
of Thoracic Surgeons. J Am Coll Cardiol. Dec 18 2012;60(24):e44-e164. PMID 23182125
5.
Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med.
Jun 14 1979;300(24):1350-1358. PMID 440357
6.
Genders TS, Steyerberg EW, Alkadhi H, et al. A clinical prediction rule for the diagnosis of coronary artery disease: validation,
updating, and extension. Eur Heart J. Jun 2011;32(11):1316-1330. PMID 21367834
©2017 Blue Cross and Blue Shield of Louisiana
Blue Cross and Blue Shield of Louisiana is an independent licensee of the Blue Cross and Blue Shield Association and incorporated
as Louisiana Health Service & Indemnity Company.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic,
mechanical, photocopying, or otherwise, without permission from Blue Cross and Blue Shield of Louisiana.
Page 17 of 21

Coronary Computed Tomography Angiography With Selective Noninvasive Fractional Flow Reserve
Policy #
00537
Original Effective Date:
02/15/2017
Current Effective Date:
10/18/2017
7.
Wasfy MM, Brady TJ, Abbara S, et al. Comparison of the Diamond-Forrester method and Duke Clinical Score to predict
obstructive coronary artery disease by computed tomographic angiography. Am J Cardiol. Apr 01 2012;109(7):998-1004. PMID
22236462
8.
Versteylen MO, Joosen IA, Shaw LJ, et al. Comparison of Framingham, PROCAM, SCORE, and Diamond Forrester to predict
coronary atherosclerosis and cardiovascular events. J Nucl Cardiol. Oct 2011;18(5):904-911. PMID 21769703
9.
Min JK, Dunning A, Gransar H, et al. Medical history for prognostic risk assessment and diagnosis of stable patients with
suspected coronary artery disease. Am J Med. Aug 2015;128(8):871-878. PMID 25865923
10.
Genders TS, Steyerberg EW, Hunink MG, et al. Prediction model to estimate presence of coronary artery disease: retrospective
pooled analysis of existing cohorts. BMJ. Jun 12 2012;344:e3485. PMID 22692650
11.
CAD Consortium. Pre-test probability of CAD. 2016; https://www.qxmd.com/calculate/calculator_287/pre-test-probability-of-cad-
12.
De Bruyne B, Fearon WF, Pijls NH, et al. Fractional flow reserve-guided PCI for stable coronary artery disease. N Engl J Med.
Sep 25 2014;371(13):1208-1217. PMID 25176289
13.
De Bruyne B, Pijls NH, Kalesan B, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N
Engl J Med. Sep 13 2012;367(11):991-1001. PMID 22924638
14.
Tonino PA, De Bruyne B, Pijls NH, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary
intervention. N Engl J Med. Jan 15 2009;360(3):213-224. PMID 19144937
15.
Pothineni NV, Shah NS, Rochlani Y, et al. U.S. trends in inpatient utilization of fractional flow reserve and percutaneous coronary
intervention. J Am Coll Cardiol. Feb 16 2016;67(6):732-733. PMID 26868697
16.
Blue Cross Blue Shield Association Technology Evaluation Center (TEC). Fractional Flow Reserve and Coronary Artery
Revascularization. TEC Assessment. June 2011;26:Tab 2.
17.
Fearon WF, Shilane D, Pijls NH, et al. Cost-effectiveness of percutaneous coronary intervention in patients with stable coronary
artery disease and abnormal fractional flow reserve. Circulation. Sep 17 2013;128(12):1335-1340. PMID 23946263
18.
van Nunen LX, Zimmermann FM, Tonino PA, et al. Fractional flow reserve versus angiography for guidance of PCI in patients
with multivessel coronary artery disease
(FAME):
5-year follow-up of a randomised controlled trial. Lancet. Nov
7
2015;386(10006):1853-1860. PMID 26333474
19.
Montalescot G, Sechtem U, Achenbach S, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the
Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. Oct
2013;34(38):2949-3003. PMID 23996286
20.
Windecker S, Kolh P, Alfonso F, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on
Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic
Surgery
(EACTS) Developed with the special contribution of the European Association of Percutaneous Cardiovascular
Interventions (EAPCI). Eur Heart J. Oct 1 2014;35(37):2541-2619. PMID 25173339
21.
Patel MR, Calhoon JH, Dehmer GJ, et al. ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2017 Appropriate Use Criteria for
coronary revascularization in patients with stable ischemic heart disease: a report of the American College of Cardiology
Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society
of Echocardiography, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society
of Cardiovascular Computed Tomography, and Society of Thoracic Surgeons. J Am Coll Cardiol. May 02 2017;69(17):2212-2241.
PMID 28291663
22.
Pijls NH, Van Gelder B, Van der Voort P, et al. Fractional flow reserve. A useful index to evaluate the influence of an epicardial
coronary stenosis on myocardial blood flow. Circulation. Dec 1 1995;92(11):3183-3193. PMID 7586302
23.
de Bruyne B, Bartunek J, Sys SU, et al. Simultaneous coronary pressure and flow velocity measurements in humans. Feasibility,
reproducibility, and hemodynamic dependence of coronary flow velocity reserve, hyperemic flow versus pressure slope index,
and fractional flow reserve. Circulation. Oct 15 1996;94(8):1842-1849. PMID 8873658
24.
HeartFlow. DEN130045, FFRct V.
1.4.
September 11, 2016.
25.
Koo BK, Erglis A, Doh JH, et al. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve
computed from coronary computed tomographic angiograms. Results from the prospective multicenter DISCOVER-FLOW
(Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) study. J Am Coll Cardiol. Nov 1
2011;58(19):1989-1997. PMID 22032711
©2017 Blue Cross and Blue Shield of Louisiana
Blue Cross and Blue Shield of Louisiana is an independent licensee of the Blue Cross and Blue Shield Association and incorporated
as Louisiana Health Service & Indemnity Company.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic,
mechanical, photocopying, or otherwise, without permission from Blue Cross and Blue Shield of Louisiana.
Page 18 of 21

Coronary Computed Tomography Angiography With Selective Noninvasive Fractional Flow Reserve
Policy #
00537
Original Effective Date:
02/15/2017
Current Effective Date:
10/18/2017
26.
Min JK, Koo BK, Erglis A, et al. Effect of image quality on diagnostic accuracy of noninvasive fractional flow reserve: results from
the prospective multicenter international DISCOVER-FLOW study. J Cardiovasc Comput Tomogr. May-Jun 2012;6(3):191-199.
PMID 22682261
27.
Nakazato R, Park HB, Berman DS, et al. Noninvasive fractional flow reserve derived from computed tomography angiography for
coronary lesions of intermediate stenosis severity: results from the DeFACTO study. Circ Cardiovasc Imaging. Nov
2013;6(6):881-889. PMID 24081777
28.
Nørgaard BL, Leipsic J, Gaur S, et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary
computed tomography angiography in suspected coronary artery disease: the NXT trial (Analysis of Coronary Blood Flow Using
CT Angiography: Next Steps). J Am Coll Cardiol. Apr 1 2014;63(12):1145-1155. PMID 24486266
29.
Taylor CA, Fonte TA, Min JK. Computational fluid dynamics applied to cardiac computed tomography for noninvasive
quantification of fractional flow reserve: scientific basis. J Am Coll Cardiol. Jun 4 2013;61(22):2233-2241. PMID 23562923
30.
Kim KH, Doh JH, Koo BK, et al. A novel noninvasive technology for treatment planning using virtual coronary stenting and
computed tomography-derived computed fractional flow reserve. JACC Cardiovasc Interv. Jan 2014;7(1):72-78. PMID 24332418
31.
HeartFlow. K152733, FFRct v2.0. 2016; https://www.accessdata.fda.gov/cdrh_docs/pdf15/K152733.pdf. Accessed September 11,
2016.
32.
Johnson NP, Johnson DT, Kirkeeide RL, et al. Repeatability of fractional flow reserve despite variations in systemic and coronary
hemodynamics. JACC Cardiovasc Interv. Jul 2015;8(8):1018-1027. PMID 26205441
33.
Hulten E, Di Carli MF. FFRCT: Solid PLATFORM or thin ice? J Am Coll Cardiol. Dec 1 2015;66(21):2324-2328. PMID 26475206
34.
Gaur S, Bezerra HG, Lassen JF, et al. Fractional flow reserve derived from coronary CT angiography: variation of repeated
analyses. J Cardiovasc Comput Tomogr. Jul-Aug 2014;8(4):307-314. PMID 25151923
35.
Nørgaard BL, Gaur S, Leipsic J, et al. Influence of coronary calcification on the diagnostic performance of CT angiography
derived FFR in coronary artery disease: a substudy of the NXT Trial. JACC Cardiovasc Imaging. Sep 2015;8(9):1045-1055. PMID
26298072
36.
Takx RA, Blomberg BA, El Aidi H, et al. Diagnostic accuracy of stress myocardial perfusion imaging compared to invasive
coronary angiography with fractional flow reserve meta-analysis. Circ Cardiovasc Imaging. Jan 2015;8(1). PMID 25596143
37.
Wu W, Pan DR, Foin N, et al. Noninvasive fractional flow reserve derived from coronary computed tomography angiography for
identification of ischemic lesions: a systematic review and meta-analysis. Sci Rep. 2016;6:29409. PMID 27377422
38.
Danad I, Szymonifka J, Twisk JWR, et al. Diagnostic performance of cardiac imaging methods to diagnose ischaemia-causing
coronary artery disease when directly compared with fractional flow reserve as a reference standard: a meta-analysis. Eur Heart
J. Apr 01 2017;38(13):991-998. PMID 27141095
39.
Renker M, Schoepf UJ, Wang R, et al. Comparison of diagnostic value of a novel noninvasive coronary computed tomography
angiography method versus standard coronary angiography for assessing fractional flow reserve. Am J Cardiol. Nov 01
2014;114(9):1303-1308. PMID 25205628
40.
De Geer J, Sandstedt M, Bjorkholm A, et al. Software-based on-site estimation of fractional flow reserve using standard coronary
CT angiography data. Acta Radiol. Oct 2016;57(10):1186-1192. PMID 26691914
41.
Min JK, Leipsic J, Pencina MJ, et al. Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. JAMA. Sep 26
2012;308(12):1237-1245. PMID 22922562
42.
Thompson AG, Raju R, Blanke P, et al. Diagnostic accuracy and discrimination of ischemia by fractional flow reserve CT using a
clinical use rule: results from the Determination of Fractional Flow Reserve by Anatomic Computed Tomographic Angiography
study. J Cardiovasc Comput Tomogr. Mar-Apr 2015;9(2):120-128. PMID 25819194
43.
Whiting PF, Rutjes AW, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy
studies. Ann Intern Med. Oct 18 2011;155(8):529-536. PMID 22007046
44.
Coenen A, Lubbers MM, Kurata A, et al. Fractional flow reserve computed from noninvasive CT angiography data: diagnostic
performance of an on-site clinician-operated computational fluid dynamics algorithm. Radiology. Mar 2015;274(3):674-683. PMID
25322342
45.
PROSPERO. International prospective register of systematic reviews. n.d.; https://www.crd.york.ac.uk/PROSPERO/.
46.
Min JK, Berman DS, Budoff MJ, et al. Rationale and design of the DeFACTO (Determination of Fractional Flow Reserve by
Anatomic Computed Tomographic AngiOgraphy) study. J Cardiovasc Comput Tomogr. Sep-Oct 2011;5(5):301-309. PMID
21930103
47.
Curzen NP, Nolan J, Zaman AG, et al. Does the routine availability of CT-derived FFR Influence management of patients with
stable chest pain compared to CT angiography alone?: The FFRCT RIPCORD Study. JACC Cardiovasc Imaging. Oct
2016;9(10):1188-1194. PMID 27568119
©2017 Blue Cross and Blue Shield of Louisiana
Blue Cross and Blue Shield of Louisiana is an independent licensee of the Blue Cross and Blue Shield Association and incorporated
as Louisiana Health Service & Indemnity Company.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic,
mechanical, photocopying, or otherwise, without permission from Blue Cross and Blue Shield of Louisiana.
Page 19 of 21

Coronary Computed Tomography Angiography With Selective Noninvasive Fractional Flow Reserve
Policy #
00537
Original Effective Date:
02/15/2017
Current Effective Date:
10/18/2017
48. Douglas PS, De Bruyne B, Pontone G, et al. 1-year outcomes of FFRCT-guided care in patients with suspected coronary
disease: the PLATFORM Study. J Am Coll Cardiol. Aug 2 2016;68(5):435-445. PMID 27470449
49. Douglas PS, Pontone G, Hlatky MA, et al. Clinical outcomes of fractional flow reserve by computed tomographic angiography-
guided diagnostic strategies vs. usual care in patients with suspected coronary artery disease: the prospective longitudinal trial of
FFR(CT): outcome and resource impacts study. Eur Heart J. Dec 14 2015;36(47):3359-3367. PMID 26330417
50. Hlatky MA, De Bruyne B, Pontone G, et al. Quality-of-life and economic outcomes of assessing fractional flow reserve with
computed tomography angiography: PLATFORM. J Am Coll Cardiol. Dec 1 2015;66(21):2315-2323. PMID 26475205
Dewey M, Rief M, Martus P, et al. Evaluation of computed tomography in patients with atypical angina or chest pain clinically
referred for invasive coronary angiography: randomised controlled trial. Bmj. Oct 24 2016;355:i5441. PMID 27777234
51. Moller Jensen J, Erik Botker H, Norling Mathiassen O, et al. Computed tomography derived fractional flow reserve testing in
stable patients with typical angina pectoris: influence on downstream rate of invasive coronary angiography. Eur Heart J
Cardiovasc Imaging. Apr 20 2017. PMID 28444153
52. Nørgaard BL, Hjort J, Gaur S, et al. Clinical use of coronary CTA-derived FFR for decision-making in stable CAD. JACC
Cardiovasc Imaging. May 2017;10(5):541-550. PMID 27085447
53. Lu MT, Ferencik M, Roberts RS, et al. Noninvasive FFR Derived From Coronary CT Angiography: Management and Outcomes in
the PROMISE Trial. JACC Cardiovasc Imaging. Apr 07 2017. PMID 28412436
54. Douglas PS, Hoffmann U, Lee KL, et al. PROspective Multicenter Imaging Study for Evaluation of chest pain: rationale and
design of the PROMISE trial. Am Heart J. Jun 2014;167(6):796-803 e791. PMID 24890527
55. National Institute for Health and Care Excellence. HeartFlow FFRCT for estimating fractional flow reserve from coronary CT
angiography [MTG32]. 2017; https://www.nice.org.uk/guidance/mtg32.
Policy History
Original Effective Date:
02/15/2017
Current Effective Date:
10/18/2017
10/05/2017
Medical Policy Committee review
10/18/2017
Medical Policy Implementation Committee approval. Policy title changed from
“Noninvasive
fractional Flow reserve Using Computed Tomography Angiography” to
“Coronary Computed
Tomography Angiography With Selective Noninvasive Fractional Flow Reserve”. Changed
coverage from investigational to eligible for coverage for individuals with stable chest pain at
intermediate risk of coronary artery disease being considered for invasive coronary angiography.
“Positive” added before CCTA to more explicitly state that FFR-CT is intended for selective use
following CCTA with positive results.
Next Scheduled Review Date:
10/2018
Coding
The five character codes included in the Blue Cross Blue Shield of Louisiana Medical Policy Coverage Guidelines are
obtained from Current Procedural Terminology (CPT®)‡, copyright 2016 by the American Medical Association (AMA).
CPT is developed by the AMA as a listing of descriptive terms and five character identifying codes and modifiers for
reporting medical services and procedures performed by physician.
The responsibility for the content of Blue Cross Blue Shield of Louisiana Medical Policy Coverage Guidelines is with
Blue Cross and Blue Shield of Louisiana and no endorsement by the AMA is intended or should be implied. The AMA
disclaims responsibility for any consequences or liability attributable or related to any use, nonuse or interpretation of
information contained in Blue Cross Blue Shield of Louisiana Medical Policy Coverage Guidelines. Fee schedules,
relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT,
and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense
medical services. The AMA assumes no liability for data contained or not contained herein. Any use of CPT outside of
Blue Cross Blue Shield of Louisiana Medical Policy Coverage Guidelines should refer to the most current Current
©2017 Blue Cross and Blue Shield of Louisiana
Blue Cross and Blue Shield of Louisiana is an independent licensee of the Blue Cross and Blue Shield Association and incorporated
as Louisiana Health Service & Indemnity Company.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic,
mechanical, photocopying, or otherwise, without permission from Blue Cross and Blue Shield of Louisiana.
Page 20 of 21

Coronary Computed Tomography Angiography With Selective Noninvasive Fractional Flow Reserve
Policy #
00537
Original Effective Date:
02/15/2017
Current Effective Date:
10/18/2017
Procedural Terminology which contains the complete and most current listing of CPT codes and descriptive terms.
Applicable FARS/DFARS apply.
CPT is a registered trademark of the American Medical Association.
Codes used to identify services associated with this policy may include (but may not be limited to) the following:
Code Type
Code
CPT
93799
HCPCS
No codes
ICD-10 Diagnosis
All related diagnoses
*Investigational - A medical treatment, procedure, drug, device, or biological product is Investigational if the effectiveness has not
been clearly tested and it has not been incorporated into standard medical practice. Any determination we make that a medical
treatment, procedure, drug, device, or biological product is Investigational will be based on a consideration of the following:
A. Whether the medical treatment, procedure, drug, device, or biological product can be lawfully marketed without approval of
the U.S. Food and Drug Administration (FDA) and whether such approval has been granted at the time the medical
treatment, procedure, drug, device, or biological product is sought to be furnished; or
B. Whether the medical treatment, procedure, drug, device, or biological product requires further studies or clinical trials to
determine its maximum tolerated dose, toxicity, safety, effectiveness, or effectiveness as compared with the standard means
of treatment or diagnosis, must improve health outcomes, according to the consensus of opinion among experts as shown
by reliable evidence, including:
1.
Consultation with the Blue Cross and Blue Shield Association technology assessment program (TEC) or other
nonaffiliated technology evaluation center(s);
2.
Credible scientific evidence published in peer-reviewed medical literature generally recognized by the relevant
medical community; or
3.
Reference to federal regulations.
**Medically Necessary (or “Medical Necessity”) - Health care services, treatment, procedures, equipment, drugs, devices, items or
supplies that a Provider, exercising prudent clinical judgment, would provide to a patient for the purpose of preventing, evaluating,
diagnosing or treating an illness, injury, disease or its symptoms, and that are:
A. In accordance with nationally accepted standards of medical practice;
B. Clinically appropriate, in terms of type, frequency, extent, level of care, site and duration, and considered effective for the
patient's illness, injury or disease; and
C. Not primarily for the personal comfort or convenience of the patient, physician or other health care provider, and not more
costly than an alternative service or sequence of services at least as likely to produce equivalent therapeutic or diagnostic
results as to the diagnosis or treatment of that patient's illness, injury or disease.
For these purposes, “nationally accepted standards of medical practice” means standards that are based on credible scientific
evidence published in peer-reviewed medical literature generally recognized by the relevant medical community, Physician Specialty
Society recommendations and the views of Physicians practicing in relevant clinical areas and any other relevant factors.
‡ Indicated trademarks are the registered trademarks of their respective owners.
NOTICE: Medical Policies are scientific based opinions, provided solely for coverage and informational purposes. Medical Policies
should not be construed to suggest that the Company recommends, advocates, requires, encourages, or discourages any particular
treatment, procedure, or service, or any particular course of treatment, procedure, or service.
©2017 Blue Cross and Blue Shield of Louisiana
Blue Cross and Blue Shield of Louisiana is an independent licensee of the Blue Cross and Blue Shield Association and incorporated
as Louisiana Health Service & Indemnity Company.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic,
mechanical, photocopying, or otherwise, without permission from Blue Cross and Blue Shield of Louisiana.
Page 21 of 21