Blue Cross Idaho
MP 6.01.59 - Coronary Computed
Tomography Angiography With Selective
Noninvasive Fractional Flow Reserve
Medical Policy
Section
Original Policy Date Last Review Status/Date
Radiology
12/2016
Reviewed with literature search/6:2017
Effective Date
Return to Medical Policy Index
7/25/2017
Disclaimer
Our medical policies are designed for informational purposes only and are not an authorization,
or an explanation of benefits, or a contract. Receipt of benefits is subject to satisfaction of all
terms and conditions of the coverage. Medical technology is constantly changing, and we
reserve the right to review and update our policies periodically.
Policy
The use of noninvasive fractional flow reserve following a positive coronary computed
tomography angiography may be considered medically necessary to guide decisions about the
use of invasive coronary angiography in patients with stable chest pain at intermediate risk of
coronary artery disease (ie, suspected or presumed stable ischemic heart disease).
The use of noninvasive fractional flow reserve not meeting the criteria outlined above is
considered investigational.
Policy Guidelines
Fractional flow reserve using coronary computed tomography angiography requires at least 64-
slice coronary computed tomography angiography and cannot be calculated when images lack
sufficient quality (HeartFlow, 2013) (11% to 13% in recent studies; Koo et al, 2011; Min et al,
2012; Nakazato et al, 2013; Nørgaard et al, 2014), eg, in obese individuals (eg, body mass
index, >35 kg/m2). The presence of dense arterial calcification or an intracoronary stent can
produce significant beam-hardening artifacts and may preclude satisfactory imaging. The
presence of an uncontrolled rapid heart rate or arrhythmia hinders the ability to obtain
diagnostically satisfactory images. Evaluation of the distal coronary arteries is generally more
difficult than visualization of the proximal and mid-segment coronary arteries due to greater
cardiac motion and the smaller caliber of coronary vessels in distal locations.
CODING
There is no specific CPT code for fractional flow reserve using coronary computed tomographic
angiography.
There is a category I CPT code for coronary computed tomographic angiography:
75574: Computed tomographic angiography, heart, coronary arteries and bypass grafts (when
present), with contrast material, including 3D image postprocessing (including evaluation of
cardiac structure and morphology, assessment of cardiac function, and evaluation of venous
Blue Cross Idaho
structures, if performed).
Benefit Application
BlueCard/National Account Issues
State or federal mandates (eg, FEP) may dictate that certain U.S. Food and Drug
Administration-approved devices, drugs, or biologics may not be considered investigational, and
thus these devices may be assessed only on the basis of their medical necessity.
Description
STABLE ISCHEMIC HEART DISEASE
Coronary artery disease (CAD) is a significant cause of morbidity and mortality and various
epidemiologic risk factors have been well studied. Evaluation of obstructive CAD involves
quantifying arterial stenoses to determine whether significant narrowing is present. Lesions with
stenosis more than 50% to 70% in diameter accompanied by symptoms are generally
considered significant. It has been suggested that coronary computed tomography angiography
(CCTA) or other noninvasive functional cardiac testing may help rule out CAD and avoid
invasive coronary angiography in patients with a low clinical likelihood of significant CAD.
However, invasive coronary angiographies (ICAs) are frequently unnecessary in patients with
suspected stable ischemic heart disease (SIHD), as evidenced by low diagnostic yields for
significant obstructive CAD. For example, from a sample of over 132,000 ICAs, Patel et al
(2010) found 48.8% of elective ICAs performed in patients with stable angina did not detect
obstructive CAD (left main stenosis ≥50% or ≥70% in a major epicardial or branch >2.0 mm in
diameter).1 ICA is clinically useful when patients with stable angina have failed optimal medical
therapy and may benefit from revascularization. A noninvasive imaging test, performed prior to
ICA as a gatekeeper, that can distinguish candidates who may benefit from early
revascularization (eg, patients with unprotected left main stenosis ≥50% or hemodynamically
significant disease) from those unlikely to benefit could avoid unnecessary invasive procedures
and their potential adverse consequences. Moreover, for the large majority of patients with
SIHD, revascularization offers no survival advantage over medical therapy; there are few who
might benefit from ICA if they have not first failed optimal medical therapy.2
Clinical Risk Prediction
The 2012 collaborative medical association guidelines for the diagnosis and management of
patients with stable heart disease list several class I recommendations on use of noninvasive
testing in patients with suspected SIHD.3 A class I recommendation indicates that a test should
be performed. In general, patients with at least intermediate risk (10%-90% risk by standard risk
prediction instruments) are recommended to have some type of test, the choice depending on
interpretability of the electrocardiogram, capacity to exercise, and presence of comorbidity.
Clinical prediction scores or models have been developed to help estimate the pretest
probability of CAD in individuals with stable chest pain. A commonly cited clinical prediction
model based on age, sex, and type of pain symptoms, originally developed by Diamond and
Forrester (1979),4 has been further studied and extended in a report by Genders et al (20115
and compared to the Duke Clinical Score by Wasfy et al (2012).6 Versteylen et al (2011)
published a comparison of clinical prediction results for the Diamond and Forrester model, the
Framingham risk score, the PROCAM risk score, and the SCORE risk estimation model.7
Another model has been published by Min et al (2015)8 and an online calculator developed by a

Blue Cross Idaho
CAD consortium.9,10
Gatekeepers to ICA
Imposing an effective noninvasive gatekeeper strategy with one or more tests before planned
ICA to avoid unnecessary procedures is compelling. The most important characteristic of a
gatekeeper test is its ability to accurately identify and exclude clinically insignificant disease
where revascularization would offer no potential benefit. From a diagnostic perspective, an
optimal strategy would result in few false-negative tests while avoiding an excessive false-
positive rate—it would provide a low posttest probability of significant disease. Such a test would
then have a small and precise negative likelihood ratio and high negative predictive value. An
effective gatekeeper would decrease the rate of ICA while increasing the diagnostic yield
(defined by the presence of obstructive CAD on ICA). At the same time, there should be no
increase in major adverse cardiac events. A clinically useful strategy would satisfy these
diagnostic performance characteristics and impact the outcomes of interest. Various tests have
been proposed as potentially appropriate for a gatekeeper function prior to planned ICA,
including CCTA, magnetic resonance imaging, single-photon emission computed tomography,
positron emission tomography, and stress echocardiography. More recently, adding noninvasive
measurement of fractional flow reserve (FFR) using CCTA has been suggested, combining
functional and anatomic information.
Fractional Flow Reserve
Invasively measured FFR evaluates the severity of ischemia caused by coronary artery
obstructions and can predict when revascularization may be beneficial.11-13 FFR has not been
used as a diagnostic test for ischemic heart disease, but as a test to evaluate the degree of
ischemia caused by a stenosis.
Invasive FFR is rarely used in the United States to guide percutaneous coronary intervention
(PCI). For example, using the National Inpatient Sample, Pothineni et al (2016) reported that
201,705 PCIs were performed in 2012, but just 21,365 FFR procedures.14 Assuming the
intention of FFR is to guide PCI, it would represent just 4.3% of PCI procedures. Whether
noninvasively obtained FFR will influence decisions concerning ICA, over and above anatomic
considerations, is therefore important to empirically establish.
Randomized controlled trials and observational studies have demonstrated that FFR-guided
revascularization can improve cardiovascular outcomes, reduce revascularizations, and
decrease costs.15 For example, the Fractional Flow Reserve versus Angiography for Multivessel
Evaluation (FAME) trial randomized 1005 patients with multivessel disease and planned
PCI.13,16 At 1 year, compared with PCI guided by angiography alone, FFR-guided PCI reduced
the number of stents placed by approximately 30%—followed by lower rates (13.2% vs 18.3%)
of major cardiovascular adverse events (myocardial infarction, death, repeat revascularization)
and at a lower cost. The clinical benefit persisted through 2 years, although by 5 years events
rates were similar between groups.17
European guidelines (2013) for stable CAD have recommended that FFR be used “to identify
hemodynamically relevant coronary lesion(s) when evidence of ischaemia is not available” (class
Ia), and “[r]evascularization of stenoses with FFR <0.80 is recommended in patients with angina
symptoms or a positive stress test.”18 Guidelines (2014) have also recommended using “FFR to
identify haemodynamically relevant coronary lesion(s) in stable patients when evidence of
ischaemia is not available” (class Ia recommendation).19 U.S. guidelines (2012) have stated that
an FFR of 0.80 or less provides level Ia evidence for revascularization for “significant stenoses
amenable to revascularization and unacceptable angina despite guideline directed medical
therapy.”3 In addition, the importance of FFR in decision making appears prominently in the
2017 appropriate use criteria for coronary revascularization in patients with SIHD.20
Blue Cross Idaho
Measuring FFR during ICA can be accomplished by passing a pressure-sensing guidewire
across a stenosis. Coronary hyperemia (increased blood flow) is then induced and pressure
distal and proximal to the stenosis is used to calculate flow across it. FFR is the ratio of flow in
the presence of a stenosis to flow in its absence. FFR levels less than 0.75 to 0.80 are
considered to represent significant ischemia while those 0.94 to 1.0 normal. Measurement is
valid in the presence of serial stenoses, is unaffected by collateral blood flow,21 and
reproducibility is high.22 Potential complications include adverse events related to catheter use
such as vessel wall damage (dissection); the time required to obtain FFR during a typical ICA is
less than 10 minutes.
FFR using CCTA requires at least 64-slice CCTA and cannot be calculated when images lack
sufficient quality23 (11% to 13% in recent studies24-27), eg, in obese individuals (eg, body mass
index, >35 kg/m2). The presence of dense arterial calcification or an intracoronary stent can
produce significant beam-hardening artifacts and may preclude satisfactory imaging. The
presence of an uncontrolled rapid heart rate or arrhythmia hinders the ability to obtain
diagnostically satisfactory images. Evaluation of the distal coronary arteries is generally more
difficult than visualization of the proximal and mid-segment coronary arteries due to greater
cardiac motion and the smaller caliber of coronary vessels in distal locations.
Noninvasive FFR Measurement
FFR can be modeled noninvasively using images obtained during CCTA28—so-called fractional
flow reserve using coronary computed tomography angiography (FFR-CT; HeartFlow software
termed FFRCT; Siemens cFFR) using routinely collected CCTA imaging data. The process
involves constructing a digital model of coronary anatomy and calculating FFR across the entire
vascular tree using computational fluid dynamics. FFR-CT can also be used for “virtual stenting”
to simulate how stent placement would be predicted to improve vessel flow.29
Only the HeartFlow FFRCT software has been cleared by the U.S. Food and Drug
Administration. Imaging analyses require transmitting data to a central location for analysis,
taking 1 to 3 days to complete. Other prototype software is workstation-based with onsite
analyses. FFR-CT requires at least 64-slice CCTA and cannot be calculated when images lack
sufficient quality23 (11% to 13% in recent studies24-27), eg, in obese individuals (eg, body mass
index, >35 kg/m2).
REGULATORY STATUS
In November 2014, FFRCT simulation software (HeartFlow) was cleared for marketing by the
U.S. Food and Drug Administration (FDA) through the de novo 510(k) process (class II, special
controls; FDA product code: PJA). In January 2016, the FFRCT v2.0 device was cleared through
a subsequent 510(k) process.
HeartFlow FFRCT postprocessing software is cleared “for the clinical quantitative and qualitative
analysis of previously acquired Computed Tomography [CT] DICOM [Digital Imaging and
Communications in Medicine] data for clinically stable symptomatic patients with coronary artery
disease. It provides FFRCT [fractional flow reserve using coronary computed tomography
angiography], a mathematically derived quantity, computed from simulated pressure, velocity
and blood flow information obtained from a 3D computer model generated from static coronary
CT images. FFRCT analysis is intended to support the functional evaluation of coronary artery
disease. The results of this analysis [FFRCT] are provided to support qualified clinicians to aid in
the evaluation and assessment of coronary arteries. The results of HeartFlow FFRCT are
intended to be used by qualified clinicians in conjunction with the patient’s clinical history,
symptoms, and other diagnostic tests, as well as the clinician’s professional judgment.”

Blue Cross Idaho
Rationale
This evidence review was originally created in December 2016 and has been updated regularly
with searches of the MEDLINE database. The most recent literature review was performed
through April 11, 2017, to identify literature assessing the potential impact of noninvasive
imaging, particularly focusing on use of coronary computed tomography angiography (CCTA)
and noninvasive fractional flow reserve (FFR), to guide use of invasive coronary angiography
(ICA) in patients with stable chest pain at intermediate risk of coronary artery disease (CAD; ie,
suspected or presumed stable ischemic heart disease [SIHD]) being considered for ICA.
HeartFlow also submitted a list of publications and materials for review.
Assessment of a diagnostic technology typically focuses on 3 categories of evidence: (1) its
technical performance (test-retest reliability or interrater reliability); (2) diagnostic accuracy
(sensitivity, specificity, and positive and negative predictive value) in relevant populations of
patients; and (3) clinical utility demonstrating that the diagnostic information can be used to
improve patient outcomes.
CCTA WITH SELECTIVE NONINVASIVE FFR
Clinical Context and Test Purpose
The purpose of selective noninvasive fractional flow reserve using coronary computed
tomography angiography (FFR-CT) in patients with stable chest pain who have suspected SIHD
and who are being considered for ICA is to select patients who may be managed safely with
observation only, instead of undergoing ICA in the short term.
The following PICOTS were used to select literature to inform this review.
Patients
The population of interest includes patients with stable chest pain at intermediate risk of CAD (ie,
with suspected or presumed SIHD) who are being considered for ICA. Patients may have
undergone prior noninvasive testing and been treated for presumed stable angina.
Interventions
The intervention of interest is CCTA with selective FFR-CT when CCTA shows evidence of
coronary artery stenosis.
Comparators
The comparator of interest is CCTA may be performed alone without FFR-CT. Individuals may
proceed directly to ICA. Conventional noninvasive imaging tests providing functional information,
including myocardial perfusion imaging (MPI) using single-photon emission computed
tomography (SPECT), stress echocardiography (SECHO), and cardiac positron emission
tomography (PET), may be used prior to ICA. Cardiovascular magnetic resonance imaging (MRI)
is also an option.
Outcomes
The final outcomes of interest include ICA rates, ICA without obstructive CAD, major adverse
cardiovascular events (MACE), and adverse events attributed to testing and treatment.
The intermediate outcome of interest is the ability of the test to distinguish clinically significant
CAD for which revascularization may provide benefit.
Timing
Rates of ICA and treatment-related morbidity are typically short-term (eg, ≤3 months). In
addition, rates of subsequent ICA, treatment-related morbidity, MACE, quality of life, and
resource utilization ascertained over a period of 1 to 3 years are also of interest.

Blue Cross Idaho
Setting
The setting is a general cardiology practice for patients undergoing nonemergent chest pain
evaluation.
Technical Performance
Data supporting technical performance derive from the test-retest reliability of FFR-CT and
invasively measured FFR (reference standard). Other technical performance considerations
were summarized in the Food and Drug Administration (FDA) documentation.23,30
Johnson et al (2015) reported on the repeatability of invasive FFR.31 Data from 190 paired
assessments were analyzed (patients measured twice over 2 minutes). The test-retest
coefficient of variation of 2.5% (r2=98.2%) was reported using a “smart minimum” in the
analyses (“the lowest average of 5 consecutive cardiac cycles of sufficient quality within a run of
9 consecutive quality beats”). Hulten and Di Carli (2015) noted that based on the Johnson
results, an FFR of 0.8 would have a 95% confidence interval (CI) of 0.76 to 0.84.32 Gaur et al
(2014) analyzed data from 28 patients (58 vessels) with repeated FFR-CT and invasive FFR
measurements.33 They reported coefficients of variation of 3.4% (95% CI, 1.5% to 4.6%) for
FFR-CT and 2.7% (95% CI, 1.8% to 3.3%) for invasive FFR. Although reproducibility was
acceptable, whether test-retest reliability over time might be similar is unclear.
The ability to obtain FFR-CT measurements is directly related to the quality of imaging data and
values are not calculated for small vessels (<1.8 mm). Nitrate administration is recommended
(generally standard practice unless contraindicated) for vasodilatation, and a lack of nitrates can
affect FFR-CT results. In addition, the FDA de novo summary lists factors that can adversely
impact FFR-CT results, including: imaging data quality, incorrect brachial pressure, myocardial
dysfunction and hypertrophy, and abnormal physiology (eg, congenital heart disease). Coronary
calcium might also impact measurements.34
Section Summary: Technical Performance
Reported results have indicated that the test-retest reliability is acceptable and other known
factors can impact variability of FFR-CT results.
Diagnostic Accuracy
Studies Included in FFR-CT Systematic Reviews: Per-Patient Diagnostic Accuracy
Twenty-six studies have contributed patient-level results to a 2015 meta-analysis that examined
5 non-FFR-CT imaging modalities (see Table 1).35 Five studies contributed results to 2 meta-
analyses, Wu et al (2016)36 and Danad et al (2017),37 evaluating the diagnostic accuracy of
FFR-CT using patients as the unit of analysis. Only the FDA-cleared HeartFlow software has
been evaluated prospectively across multiple sites. Two small retrospective studies have
reported per-patient performance characteristics for the prototype Siemens workstation-based
software.38,39 The 3 HeartFlow FFRCT studies used successive software versions with reported
improvement in specificity (from 54% to 79%) between versions 1.2 and 1.4.24,27,40 The NXT
Trial, the basis for device clearance by FDA, was conducted at 11 sites in 8 countries (Canada,
EU, Asia).27 Although not examined in the 2 included meta-analyses, subgroup analyses
suggested little variation in results by sex and age.41 Effectively, the entirety of the data was
obtained in patients of white or Asian decent; almost all patients were appropriate for testing
according to FDA clearance.
Danad et al
Danad et al (2017) included 23 studies published between January 2002 and February 2015
evaluating the diagnostic performance of CCTA, FFR-CT, SPECT, SECHO, MRI, or ICA
compared with an invasive FFR reference standard.37 The 3 included FFR-CT studies used the
HeartFlow software and had performed FFR in at least 75% of patients. A cutoff of 0.75 defined

Blue Cross Idaho
significant stenosis in 8 (32%) studies and in the remainder 0.80 (the current standard used in all
FFR-CT studies). Per-patient and per-vessel meta-analyses were performed. Study quality was
assessed using QUADAS-242; no significant biases were identified in FFR-CT studies but a high
risk of biased patient selection was judged in 10 (43.4%) of other studies. HeartFlow funded
publication Open Access; 1 author was a consultant to, and another a cofounder of, HeartFlow.
On the patient level, MRI had the highest combined sensitivity (90%; 95% CI, 75% to 97%) and
specificity (94%; 95% CI, 79% to 99%) for invasive FFR, but were estimated from only 2 studies
(70 patients). FFR-CT had similar sensitivity (90%; 95% CI, 85% to 93%), but lower specificity
(71%; 95% CI, 65% to 75%), and accordingly a lower positive likelihood ratio (3.34; 95% CI, 1.78
to 6.25) than MRI (10.31; 95% CI, 3.14 to 33.9). The negative likelihood ratios were low (lower is
better) for both FFR-CT (0.16; 95% CI, 0.11 to 0.23) and MRI (0.12; 95% CI, 0.05 to 0.30);
however, the confidence interval is more narrow for FFR-CT due to larger sample for FFR-CT.
CCTA had a slightly higher negative likelihood ratio (0.22; 95% CI, 0.10 to 0.50). Results for the
per-vessel area under the summary receiver operating characteristic curve were similar except
for CCTA where per-patient results were considerably worse (eg, C statistic of 0.57 vs. 0.85).
Reviewers noted heterogeneity in many estimates (eg, CCTA sensitivity, I2=80%). Finally,
pooled results for some imaging tests included few studies.
Wu et al
Wu et al (2016) identified 7 studies (833 patients, 1377 vessels) comparing FFR-CT with
invasively measured FFR from searches of PubMed, Cochrane, EMBASE, Medion, and meeting
abstracts through January 2016.36 Studies included patients with established or suspected
SIHD. In addition to the 3 FFR-CT studies pooled by Danad et al, 1 additional study using
HeartFlow technique (44 patients; 48 vessels) and 3 additional studies (180 patients; 279
vessels) using Siemens cFFR software (not FDA approved or cleared) were identified. An
invasive FFR cutoff of 0.80 was the reference standard in all studies. Per-patient results
reported in 5 studies were pooled and reported in Table 1. All studies were rated at low risk of
bias and without applicability concerns using the QUADAS-2 tool.42 Appropriate bivariate meta-
analyses (accounting for correlated sensitivity and specificity) were used.
As expected given study overlap, FFR-CT performance characteristics were similar to those
reported by Danad et al, but with a slightly higher specificity (see Table 1). The pooled per-
vessel C statistic was lower (0.86) than the per-patient result (0.90). No evidence of publication
bias was detected, but the number of studies was too small to adequately assess. Reviewers
noted that, in 2 studies, FFR-CT results were uninterpretable in 12.0%27 and 8.2%43 of
participants.
Takx et al
Takx et al (2015) identified studies reporting on the ability of perfusion computed tomography
(CT), MRI, SECHO, PET, and SPECT to detect hemodynamically significant CAD as measured
by ICA with invasive FFR.35 Studies published through May 2014 were eligible for inclusion;
PubMed, EMBASE, and Web of Science were searched. QUADAS-2 was used to assess study
quality42; studies generally rated poorly on blinding of the index test result from the assessor and
study population selection. Reviewers designated the negative likelihood ratio as the diagnostic
characteristic of interest (ie, ability to exclude disease) noting that MPI (eg, MRI, SPECT, PET,
or CT) has been proposed to be a gatekeeper to ICA. No funding was obtained for the review
and the study was registered on PROSPERO44 (the 2 other meta-analyses were not).
The pooled negative likelihood ratios for MRI, PET, and perfusion CT were similar in magnitude
(0.12 to 0.14; see Table 1) although the confidence interval for PET was wide. Heterogeneity
among studies included in the pooled patient-level results was considered high for PET
(I2=84%), moderate for CT (I2=70%) and SPECT (I2=55%), and low for MRI (I2=0%) and
SECHO (I2=0%). Publication bias, when able to be assessed, was not suspected. With respect

Blue Cross Idaho
to ability to detect hemodynamically significant ischemia, reviewers concluded that “MPI with
MRI, CT, or PET has the potential to serve as a gatekeeper for invasive assessment of
hemodynamic significance by ICA and FFR.” Studies of FFR-CT were not included in the
analysis.
Table 1. Pooled Per-Patient Pooled Diagnostic Performance of Noninvasive Tests for
Invasive FFR
Sensitivity
Specificity
LR+
LR-
Test
Studies N
C
(95% CI)
(95% CI)
(95% CI) (95% CI)
Danad et al
(2017)37
10.3
0.12
90% (75 to
94% (79 to
MRI
2
70
0.94
(3.14 to
(0.05 to
97)
99)
33.9)
0.30)
0.16
90% (85 to
71% (65 to
3.3
(1.78
FFR-CT 3
609
0.94
(0.11 to
93)
75)
to 6.25)
0.23)
0.22
90% (86 to
39% (34 to
1.5
(1.25
CCTA
4
694
0.57
(0.10 to
93)
44)
to 1.90)
0.50)
0.34
77% (61 to
75% (63 to
3.0
(1.94
SECHO 2
115
0.82
(0.17 to
88)
85)
to 4.65)
0.66)
0.40
70% (59 to
78% (68 to
3.4
(1.04
SPECT 3
110
0.79
(0.19 to
80)
87)
to 11.1)
0.83)
0.46
69% (65 to
67% (63 to
2.5
(1.25
ICA
2
954
0.75
(0.39 to
75)
71)
to 5.13)
0.55)
Wu et al
(2016)36
0.14
89% (85 to
76% (64 to
3.7
(2.41
FFR-CT 5
833
0.90
(0.09 to
93)
84)
to 5.61)
0.21)
35
Takx et al (2015)
0.14
89% (86 to
87% (83 to
6.3
(4.88
MRI
10
798
0.94
(0.10 to
92)
90)
to 8.12)
0.18)
0.12
88% (82 to
80% (73 to
3.8
(1.94
PCT
5
316
0.93
(0.04 to
92)
86)
to 7.40)
0.33)
0.42
69% (56 to
84% (75 to
3.7
(1.89
SECHO 4
177
0.83
(0.30 to
79)
90)
to 7.15)
0.59)
0.39
74% (67 to
79% (74 to
3.1
(2.09
SPECT 8
533
0.82
(0.27 to
79)
83)
to 4.70)
0.55)
0.14
84% (75 to
87% (80 to
6.5
(2.83
PET
2
224
0.93
(0.02 to
91)
92)
to 15.1)
0.87)

Blue Cross Idaho
CCTA: coronary computed tomography angiography; CI: confidence interval; FFR-CT: fractional
flow reserve using coronary computed tomography angiography; ICA: invasive coronary
angiography; LR: likelihood ratio; MRI: magnetic resonance imaging; PCT: perfusion computed
tomography; PET: positron emission tomography; SECHO: stress echocardiography; SPECT:
single-photon emission computed tomography.
Section Summary: Diagnostic Accuracy
Three studies including 609 patients have evaluated diagnostic accuracy of the FDA-cleared
HeartFlow software. Software used in successive studies was also revised to improve
performance characteristics, particularly specificity. For example, using an earlier software
version, the DeFACTO Trial reported a specificity of 54%.45 Accordingly, pooled results from the
Danad systematic review must be interpreted carefully. In addition, there is some uncertainty in
the generalizability of results obtained in these studies conducted under likely controlled
conditions (eg, data from the NXT Trial27 forming the basis for FDA clearance).
Given the purpose to avoid ICA, the negative likelihood ratio, or how a negative result might
dissuade a clinician from proceeding to ICA, is of primary interest—ie, excluding a patient with
vessels having a high FFR from ICA. While confidence intervals are relatively wide and
overlapping, the negative likelihood ratio estimates of FFR-CT for excluding physiologically
significant coronary stenoses tended to be lower (ie, better) than CCTA alone, SECHO, SPECT,
and ICA. Only MRI yielded a similarly low or lower negative likelihood ratio than FFR-CT.
Clinical Utility
Indirect Evidence
Diagnostic performance can offer indirect evidence of clinical utility, assuming providers act
according to a test result. As previously noted, an effective gatekeeper strategy must be able to
decrease the probability of disease (rule out) sufficiently that a planned ICA would not be
performed. Ruling out disease is a function of the negative likelihood ratio that defines the
degree to which a negative test decreases the posttest odds (and probability) of disease. The
steps in the logic are illustrated in Figure 1.
Figure 1. Pathway for Clinical Use of FFR-CT to Support Clinical Utility
FFR-CT: fractional flow reserve using coronary computed tomography angiography.
Table 2 illustrates how a negative test would lower the probability of a hemodynamically
significant obstruction from pretest probabilities of 0.25, 0.50, or 0.75 for the various tests
examined in the meta-analyses. For example, according to the results of Danad et al, if the
pretest probability was 0.50, following a negative CCTA study the posttest probability would be
0.18 (95% CI, 0.09 to 0.33); and following a negative SECHO, 0.25 (95% CI, 0.15 to 0.40) or
SPECT, 0.29 (95% CI, 0.16 to 0.45). In contrast, beginning with a pretest probability of 0.50, a
negative FFR-CT would yield a posttest probability of 0.14 (95% CI, 0.10 to 0.19) (Danad et al)
and 0.12 (95% CI, 0.08 to 0.17) (Wu et al). Overall, the negative likelihood ratios and posttest
probability estimates for FFR-CT are slightly better than CCTA as well as SECHO and SPECT.
Table 2. Change in Disease Probability Following a Negative Test
Posttest Probability (95% CI) After
Negative Test
Pretest
Pretest
Negative Pretest
Probability Probability
LR (95% Probability
Study Modality

Blue Cross Idaho
CI)
0.2
Posttest Probability (95% CI) After
Negative Test
Danad
et al
(2016)
0.12
(0.05
0.04
(0.02
0.11
(0.05
0.26
(0.13
MRI
to 0.30)
to 0.09)
to 0.23)
to 0.47)
0.16
(0.11
0.05
(0.04
0.14
(0.10
0.32
(0.25
FFR-CT
to 0.23)
to 0.07)
to 0.19)
to 0.41)
0.22
(0.10
0.07
(0.03
0.18
(0.09
0.40
(0.23
CCTA
to 0.50)
to 0.14)
to 0.33)
to 0.60)
0.34
(0.17
0.10
(0.05
0.25
(0.15
0.50
(0.34
SECHO
to 0.66)
to 0.18)
to 0.40)
to 0.66)
0.40
(0.19
0.12
(0.06
0.29
(0.16
0.55
(0.36
SPECT
to 0.83)
to 0.22)
to 0.45)
to 0.71)
0.46
(0.39
0.13
(0.12
0.32
(0.28
0.58
(0.54
ICA
to 0.55)
to 0.15)
to 0.35)
to 0.62)
Wu et al
(2016)
0.14
(0.09
0.04
(0.03
0.12
(0.08
0.30
(0.21
FFR-CT
to 0.21)
to 0.07)
to 0.17)
to 0.39)
Takx et
al (2015)
0.14
(0.10
0.04
(0.03
0.12
(0.09
0.30
(0.23
MRI
to 0.18)
to 0.06)
to 0.15)
to 0.35)
Perfusion
0.12
(0.04
0.04
(0.01
0.11
(0.04
0.26
(0.11
CT
to 0.33)
to 0.10)
to 0.25)
to 0.50)
0.42
(0.30
0.12
(0.09
0.30
(0.23
0.56
(0.47
SECHO
to 0.59)
to 0.16)
to 0.37)
to 0.64)
0.39
(0.27
0.12
(0.08
0.28
(0.21
0.54
(0.45
SPECT
to 0.55)
to 0.15)
to 0.35)
to 0.62)
0.14
(0.02
0.04
(0.01
0.12
(0.02
0.30
(0.06
PET
to 0.87)
to 0.22)
to 0.47)
to 0.72)
CCTA: coronary computed tomography angiography; CI: confidence interval; CT: computed
tomography; FFR-CT: fractional flow reserve using coronary computed tomography
angiography; ICA: invasive coronary angiography; LR: likelihood ratio; MRI: magnetic resonance
imaging; PET: positron emission tomography; SECHO: stress echocardiography; SPECT:
single-photon emission computed tomography.

Blue Cross Idaho
We identified 1 study (Curzen et al, 2016) that examined 200 consecutive individuals selected
from the NXT trial population “to reproduce the methodology of the invasive RIPCORD study”
with elective management of stable chest pain.46 All subjects received CCTA including FFR-CT
“in at least 1 vessel with diameter ≥ 2 mm and diameter stenosis ≥ 30%” as well as ICA within 60
days of CCTA. Three experienced interventional cardiologists reviewed the CCTA results
(initially without the FFR-CT results) and selected a management plan from the following 4
options: “1) optimal medical therapy (OMT) alone; 2) PCI + OMT; 3) coronary artery bypass graft
+ OMT; or 4) more information about ischemia required - they committed to option 1 by
consensus.” Following the initial decision, results from the FFR-CT were shared with the same
group of interventional cardiologists who again made a decision by consensus based on the
same 4 options. A cutoff of 0.80 or less was considered significant on FFR-CT. A stenosis was
considered significant on CCTA or ICA with 50% or more diameter narrowing. Change in
management between the first decision based on CCTA only and the second decision based on
CCTA plus FFR-CT was the primary end point of this study. Secondary end points included
analysis of the vessels considered to have significant stenosis based on CCTA alone versus
CCTA plus FFR-CT as well as vessels identified as targets for revascularization based on CCTA
alone versus CCTA plus FFR-CT. This study was conducted by investigators in the United
Kingdom and Denmark. Funding was provided by HeartFlow and multiple authors reported
receiving fees, grants, and/or support from HeartFlow.
Results for the primary end point (see Table 3) yielded a change in management category for 72
of 200 (36%) individuals. For the 87 individuals initially assigned to PCI based on CCTA alone,
the addition of the FFR-CT results shifted management for 26 of 87 (30%) to OMT (ie, no
ischemic lesion on FFR-CT) and an additional 16 (18%) individuals remained in the PCI category
but FFR-CT identified a different target vessel for PCI. These findings provide supportive
information that the improved diagnostic accuracy of FFR-CT in particular related to its better
negative likelihood ratio compared to CCTA alone would likely lead to changes in management
that would be expected to improve health outcomes.
Table 3. Summary of Overall Changes to Management in Patients Using CCTA vs CCTA +
FFR-CT
CCTA
CCTA + FFR-
Strategy
Management Category Alone,
CT,
Changea (95%
Consensus Decision
CI)
n (%)
n (%)
More data required
38 (19.0%)
0
-
23% (18% to
Optimal medical therapy
67 (33.5%)
113 (56.5%)
29%)
Percutaneous coronary
-5% (-2% to -
87 (43.5%)
78 (39.0%)
intervention
8%)
Coronary artery bypass
0.5% (0.1% to
8 (4.0%)
9 (4.5%)
graft surgery
3%)
CCTA: coronary computed tomography angiography; CI: confidence interval; FFR-CT: fractional
flow reserve using coronary computed tomography angiography.
a p<0.001 for between-group change, CCTA alone vs CCTA + FFR-CT.
Direct Evidence
We identified 2 prospective comparative studies including 1 prospective nonrandomized study
that compared an FFR-CT strategy (CCTA with noninvasive FFR measurement when requested
or indicated) with ICA and 1 randomized controlled trial that examined CCTA as a gatekeeper to
ICA (see Tables 4 and 5). In addition, we identified 1 prospective cohort study and 2

Blue Cross Idaho
retrospective cohort studies of patients referred for CCTA, which included FFR-CT evaluation.
PLATFORM Study
The Prospective LongitudinAl Trial of FFRCT: Outcome and Resource Impacts (PLATFORM)
study compared diagnostic strategies with or without FFR-CT in patients with suspected stable
angina but without known CAD.47,48 The study was conducted at 11 EU sites. All testing was
nonemergent. Patients were divided into 2 strata, according to whether the test planned prior to
study enrollment was: (1) noninvasive or (2) ICA (the patient population of interest in this
evidence review). Patients were enrolled in consecutive cohorts, with the first cohort undergoing
a usual care strategy followed by a second cohort provided CCTA with FFR-CT performed when
requested (recommended if stenoses ≥30% were identified). Follow-up was scheduled at 90
days and 6 and 12 months after entry (99.5% of patients had 1-year follow-up data). Funding
was provided by HeartFlow and multiple authors reported receiving fees, grants, and/or support
from HeartFlow. Data analyses were performed by the Duke Clinical Research Institute.
ICA without obstructive disease at 90 days was the primary end point in patients with planned
invasive testing—“no stenosis ≥ 50% by core laboratory quantitative analysis or invasive FFR <
0.80.” Secondary end points included ICA without obstructive disease following planned
noninvasive testing, and (1) MACE at 1 year defined as a composite of all-cause mortality,
myocardial infarction (MI), and urgent revascularization and (2) MACE and vascular events
within 14 days. Quality of life (QOL) was evaluated using the Seattle Angina Questionnaire, and
EQ-5D (5-item and 100-point visual analog scale). CCTA studies were interpreted by site
investigators; quantitative coronary angiography measurements were performed at a central
laboratory, as was FFR-CT. Cumulative radiation was also assessed. A sample size of 380
patients in the invasive strata yielded a 90% power to detect a 50% decrease in the primary end
point given a 30% event rate (ICA without obstructive disease) with a usual care strategy and a
dropout rate up to 10%.
ICA was planned in 380 participants, of whom 193 (50.8%) had undergone prior noninvasive
testing. The mean pretest probability in the planned ICA strata was approximately 50% (51.7%
and 49.4% in the 2 groups). FFR-CT was requested in 134 patients and successfully obtained in
117 of 134 (87.3%) in the FFR-CT group. At 90 days, 73.3% of those in the usual care group
had no obstructive findings on ICA compared with 12.4% in the FFR-CT group based on core
laboratory readings (56.7% and 9.3% based on site readings). The difference was similar in a
propensity-matched analysis of a subset of participants (n=148 from each group or 78% of the
entire sample). Prior noninvasive testing did not appear associated with nonobstructive findings.
MACE rates were low and did not differ between strategies. Mean level of radiation exposure
though 1 year was also similar in the usual care group (10.4 mSv) and the planned ICA group
(10.7 mSv). No differences in QOL were found between groups.49
Results of the PLATFORM study support the notion that, in patients with planned ICA, FFR-CT
can decrease the rate of ICAs and unnecessary procedures (finding no significant obstructive
disease) and that FFR-CT may provide clinically useful information to physicians and patients.
Study limitations include a nonrandomized design; high rate of no obstructive disease with a
usual care strategy (73.3%), which was higher than the 30% rate assumed in the sample size
estimates; and a sample size that was small with respect to evaluating adverse cardiac events.
Although finding a large effect in patients with planned invasive testing, the nonrandomized
design limits causal inferences and certainty that the magnitude of effect. The propensity-
matched analysis (in a matched subset) offers some reassurance, but the sample size was likely
too small to provide robust results.
CAD-Man Trial
Dewey et al (2016) conducted the Coronary Artery Disease Management (CAD-Man) trial, a
single-center, parallel-group assignment trial examining CCTA as a gatekeeper to ICA in patients
with atypical angina or chest pain and suspected CAD who were indicated for ICA.50 Patients

Blue Cross Idaho
were randomized to direct ICA or to ICA only if a prior CCTA was positive (a stenosis ≥70%
stenosis in any vessel or ≥50% in the left main coronary artery). The trialists reported that when
obstructive disease was suspect following CCTA, late enhancement MRI was performed to
evaluate the extent of viable myocardium (completed in 17 patients) to guide revascularization;
however, the study protocol clarified that MRI was not used for decisions to proceed to ICA. A
major procedural complication (death, stroke, MI, or event requiring >24-hour hospitalization)
within 24 hours was the primary outcome; secondary outcomes included ICA with obstructive
CAD (diagnostic yield), revascularizations, and MACE during long-term follow-up. The trial was
performed in Germany. Patients were excluded if they had evidence of ischemia or signs of MI
and just over half (56.5%) were inpatients at the time of enrollment. Obstructive disease was
defined as “at least one 50% diameter stenosis in the left main coronary artery or at least one
70% diameter stenosis in other coronary arteries.” Allocation concealment appeared adequate,
but the trial was unblinded owing to the nature of the intervention. In addition, the mean pretest
probability of CAD at baseline was higher in the ICA-only arm (37.3% vs. 31.3%; see Table 4).
The research was supported by public funding.
ICAs were reduced by 85.6% in the CCTA arm and by 80.9% for ICA with no obstructive
disease. A major procedural complication (the primary outcome) occurred in a single patient
undergoing CCTA. PCIs were less frequent when CCTA was performed—9.6% versus 14.2%
(p<0.001). Over a median follow-up of 3.3 years, MACE rates were similar in the trial arms
(4.2% in the CCTA group vs 3.7% with ICA; adjusted hazard ratio [HR], 0.90; 95% CI, 0.30 to
2.69). In the CCTA arm, there was 1 death, 2 patients with unstable angina, and 6
revascularizations; in the ICA arm there was 1 MI, 1 stroke, and 5 revascularizations.
The trial demonstrated that CCTA as a gatekeeper to planned ICA can avoid a large number of
procedures, a corresponding increase in the diagnostic yield, and fewer revascularizations. Of
note, the prevalence of obstructive CAD found on ICA in this study population was 13% (43/334
eligible for primary outcome analysis), which is lower than the prevalence of obstructive CAD in
the PLATFORM population (26.7%). Thus, the subset of individuals who went onto ICA following
CCTA findings of obstructive CAD was 20 (12%) of 167 eligible for primary outcome analysis
and only 3 (1.7%) were found to have no obstructive CAD on ICA. MACE rates did not differ
between arms. The trial was powered neither to detect a difference nor to assess noninferiority—
implications of the absence of a difference are limited. Finally, although the patient population
included those scheduled for elective ICA, it was heterogeneous, including those with recent
onset and longer standing chest pain. The single-center nature of the trial is an additional
limitation; a subsequent multicenter trial (DISCHARGE) is ongoing.
Table 4. Characteristics of Comparative Studies
Characteristics
Nonrandomized
Randomized
PLATFORM
CAD-Man
ICA
FFR-CT ICA
CCTA
(n=187)
(n=193)
(n=162)
(n=167)
60.4
Age (SD), y
63.4
(10.9)
60.7
(10.2)
60.4
(11.4)
(11.3)
Female, n (%)
79 (42.2%)
74 (38.3%)
88 (52.7%)78
(48.1%)
Race/ethnic minority, n
2 (1.1%)
1 (0.5%)
(%)
Pretest probability
51.7%
49.4%
37.3%
31.3%

Blue Cross Idaho
obstructive CAD, % (SD) (16.7%)
(17.2%)
(24.8%)
(21.1%)
Angina (%)
Typical
52 (27.8%)
45 (23.3%)
122
Atypical
142 (73.6%) 79 (48.8%)65
(65.2%)
(38.9%)
Noncardiac
12 (7.0%)
5 (2.6%)
80 (49.4%)97
(58.1%)
Other chest discomfort
3 (1.8%)
5 (3.0%)
Prior noninvasive
92 (49.2%)
101 (52.3%) 84 (50.3%)92
testing, n (%)
(56.8%)
Diabetes, n (%)
36 (19.3%)
30 (15.5%)
30 (18.5%) 15 (9.0%)
Current smoker
34 (21.0%)
41 (24.5%)
103
Current or past smoker
101 (52.3%) 85 (52.4%)88
(55.1%)
(52.6%)
CAD: coronary artery disease; CCTA: coronary computed tomography angiography; FFR-CT:
fractional flow reserve using coronary computed tomography angiography; ICA: invasive
coronary angiography.
Table 5. Results of Comparative Studies
Outcomes
Nonrandomized
Randomized
PLATFORM
CAD-Man
ICA
FFR-CT ICA
CCTA
(n=187)
(n=193)
(n=162)
(n=167)
Noninvasive FFR-CT
134
Requested, n (%)
(69.4%)
Successfully
117
performed, n (%)
(60.1%)
ICA no obstructive
137
24
6
137 (84.5%)
disease, n (%)
(73.3%)
(12.4%)
(3.6%)
Absolute difference
60.8% (53.0% to
80.9% (74.6% to 87.2%)
(95% CI), %
68.7%)
187
76
162
ICA, n (%)
24 (14.4%)
(100%)
(39.4%)
(100%)
Absolute difference
60.6% (53.7% to
85.6% (80.3% to 90.9%)
(95% CI), %
67.5%)
Revascularization, n

Blue Cross Idaho
Outcomes
Nonrandomized Randomized
49
55
PCI
(26.2%)
(28.5%)
CABG
18 (9.6%) 10 (5.2%)
67
65
16
Any
23 (14.2%)
(35.8%)
(33.7%)
(9.6%)
1-year outcomes, n
(%)
MACEa
2 (1.1%)
2 (1.0%)
MACEb
6 (3.7%)
7 (4.2%)
CABG: coronary artery bypass grafting; CI: confidence interval; FFR-CT: fractional flow reserve
using coronary computed tomography angiography; ICA: invasive coronary angiography; MACE:
major adverse cardiovascular events; PCI: percutaneous coronary intervention.
a Death, myocardial infarction, unplanned urgent revascularization
b Cardiac death, myocardial infarction, stroke, unstable angina, any revascularization.
Møller Jensen et al Prospective Cohort
Møller Jensen et al (2017) reported on a single-institution study of 774 consecutive individuals
with suspicion of CAD referred for nonemergent ICA or CCTA.51 Subjects were analyzed in 2
groups: a low-intermediate-risk group accounting for 76% of patients with mean pretest
probability of CAD 31% and a high-risk group accounting for 24% of patients with mean pretest
probability of CAD 67%. Among the 745 who received CCTA, FFR-CT was selectively ordered in
28% of patients overall (23% in the low-intermediate-risk group, 41% in the high-risk group).
CCTA was considered inconclusive in 3% of subjects and among those with conclusive CCTA,
FFR-CT yielded few inconclusive results, with less than 3% of cases. During a minimum 90-day
follow-up, the combined testing strategy of selective FFR-CT following CCTA resulted in
avoiding ICA in 91% of low-intermediate-risk and 75% of high-risk individuals. None of the
patients who avoided ICA based on CCTA with selective FFR-CT were associated with serious
clinical adverse events over an average of 157 days of follow-up.
Nørgaard et al Retrospective Cohort
Nørgaard et al (2017) reported on results from symptomatic patients referred for CCTA at a
single center in Denmark from May 2014 to April 2015.52 All data were obtained from medical
records and registries; the study was described as a “review” of diagnostic evaluations and
apparently retrospectively conducted. Follow-up through 6 to 18 months was ascertained. From
1248 referred patients, 1173 underwent CCTA; 858 received medical therapy, 82 underwent
ICA, 44 MPI, and 189 FFR-CT (185 [98%] obtained successfully). Of the 185 individuals who
successfully obtained FFR-CT, FFR-CT demonstrated values of 0.80 or less in 1 or more
vessels in 57 (31%) patients and 49 (86%) went on to ICA; whereas of the 128 with higher FFR-
CT values, only 5 (4%) went on to ICA. Assuming ICA was planned for all patients undergoing
FFR-CT, these results are consistent with FFR-CT being able to decrease the rate of ICA.
However, implications are limited by the retrospective design, performance at a single center,
and lack of a comparator arm including one for CCTA alone.
Lu et al Retrospective Cohort
Lu et al (2017) retrospectively examined a subgroup referred to ICA53 from the completed
PROspective Multicenter Imaging Study for Evaluation of Chest Pain (PROMISE) trial.

Blue Cross Idaho
PROMISE was a pragmatic trial comparing CCTA with functional testing for the initial evaluation
of patients with suspected SIHD.54 Of 550 participants referred to ICA within 90 days, 279 were
not considered for the analyses due to CCTA performed without nitroglycerin (n=139), CCTA not
meeting slice thickness guidelines (n=90), or nondiagnostic studies (n=50). Of the remaining 271
patients, 90 scans were inadequate to obtain FFR-CT, leaving 181 (33%) of those referred to
ICA for analysis. Compared with those excluded, patients in the analytic sample were less often
obese, hypertensive, diabetic, minority, or reported a CAD equivalent symptom. The 2 groups
had similar pretest probabilities of disease, revascularization rates, and MACE, but the
distribution of stenoses in the analytic sample tended to be milder (p=0.06). FFR-CT studies
were performed in a blinded manner and not available during the conduct of PROMISE for
decision making.
Severe stenoses (≥70%) or left main disease (≥50%) were present in 110 (66%) patients by
CCTA result and in 54% by ICA. Over a 29-month median follow-up, MACE (death, nonfatal MI,
hospitalization for unstable angina) or revascularization occurred in 51% of patients (9% MACE,
49% revascularization). A majority (72%) of the sample had at least 1 vessel with an FFR-CT
≤0.80, which was also associated with a higher risk of revascularization but with a wide
confidence interval (HR = 5.1; 95% CI, 2.6 to 11.5). If reserved for patients with an FFR-CT of
0.80 or less, ICAs might have been avoided in 50 patients (ie, reduced by 28%) and the rate of
ICA without 50% or more stenosis from 27% (calculated 95% CI, 21% to 34%) to 15%
(calculated 95% CI, 10% to 23%). If the 90 patients whose images sent for FFR-CT but were
unsatisfactory proceeded to ICA—as would have occurred in practice—the rate of ICA might
have decreased by 18% and ICA without significant stenosis from 31% to 25%.
The authors suggested that when CCTA is used as the initial evaluation for patients with
suspected SIHD, adding FFR-CT could have decreased the referral rate to ICA in PROMISE
from 12.2% to 9.5%, or close to the 8.1% rate observed in the PROMISE functional testing arm.
They also noted similarity of their findings to PLATFORM and concluded, “In this hypothesis-
generating study of patients with stable chest pain referred to ICA after [C]CTA, we found that
adding FFRCT may improve the efficiency of referral to ICA, addressing a major concern of an
anatomic [C]CTA strategy. FFRCT has incremental value over anatomic [C]CTA in predicting
revascularization or major adverse cardiovascular events.”
This retrospective observational subgroup analysis from PROMISE suggests that when CCTA is
the initial noninvasive test for the evaluation of suspected SIHD, FFR-CT prior to ICA has the
potential to reduce unnecessary ICAs and increase the diagnostic yield. However, study
limitations and potential generalizability are important to consider. First, analyses included only a
third of CCTA patients referred to ICA and the some characteristics of the excluded group
differed from the analytic sample. Second, conclusions assume that an FFR-CT greater than
0.80 will always dissuade a physician from recommending ICA and even in the presence of
severe stenosis (eg, ≥70% in any vessel or ≥50% in the left main)—or almost half (46%) of
patients with an FFR-CT greater than 0.80. Finally, estimates including patients with either
nondiagnostic CCTA studies (n=50) or studies inadequate for calculating FFR-CT (n=90) are
more appropriate because most likely those patients would proceed in practice to ICA.
Accordingly, the estimates are appropriately considered upper bounds for what might be seen in
practice. It is also important to note that in strata of the PLATFORM trial enrolling patients for
initial noninvasive testing (not planned ICA), ICA was more common following CCTA and
contingent FFR-CT than following usual care (18.3% vs. 12.0%) and ICA, with no obstructive
disease more frequent in the FFR-CT arm (12.5% vs. 6.0%).
Section Summary: Clinical &tility
The evidence on the diagnostic performance characteristics, particularly showing higher
specificity of FFR-CT and better negative likelihood ratio as compared to CCTA alone, may be
combined with indirect evidence that CCTA with a selective FFR-CT strategy would likely lead to
changes in management that would be expected to improve health outcomes, particularly by

Blue Cross Idaho
limiting unnecessary invasive coronary angiography testing. Moreover, there is direct evidence,
provided by 2 prospective and 2 retrospective studies, that compares health outcomes observed
during 90-day to 1-year follow-up for strategies using CCTA particularly in combination with
selective FFR-CT with strategies using ICA or other noninvasive imaging tests. The available
evidence provides support that use of CCTA with selective FFR-CT is likely to reduce the use of
ICA in individuals with stable chest pain who are unlikely to benefit from revascularization by
demonstrating the absence of functionally significant obstructive CAD. In addition, the benefits
are likely to outweigh potential harms given that rates of revascularization for functionally
significant obstructive CAD appear to be similar and cardiac-related adverse events do not
appear to be increased following a CCTA with selective FFR-CT strategy. While individual
studies are noted to have specific methodologic limitations and some variation is noted in the
magnitude of benefit across studies, in aggregate the evidence provides reasonable support that
the selective addition of FFR-CT following CCTA results in a meaningful improvement in the net
health outcome.
SUMMARY OF EVIDENCE
For individuals with stable chest pain at intermediate risk of coronary artery disease (CAD; ie,
suspected or presumed stable ischemic heart disease) being considered for invasive coronary
angiography (ICA) who receive noninvasive fractional flow reserve (FFR) measurement following
positive coronary computed tomography angiography (CCTA), the evidence includes both direct
and indirect evidence: 2 meta-analyses on diagnostic performance; 1 prospective, multicenter
nonrandomized comparative study; 1 prospective cohort; 2 retrospective cohort studies; and a
study reporting changes in management associated with CCTA-based strategies with selective
addition of fractional flow reserve using coronary computed tomography angiography (FFR-CT)
and a randomized controlled trial (RCT) of CCTA alone compared with ICA. Relevant outcomes
are test accuracy and validity, morbid events, quality of life, resource utilization, and treatment-
related morbidity. The meta-analyses indicated that CCTA has high sensitivity but moderately
low specificity for hemodynamically significant obstructive disease. Given the available evidence
that CCTA alone has been used to select patients to avoid ICA, the studies showing higher
specificity of FFR-CT and lower negative likelihood ratio of FFR-CT compared with CCTA alone,
may be used to build a chain of evidence that CCTA with a selective FFR-CT strategy would
likely lead to changes in management that would be expected to improve health outcomes by
further limiting unnecessary ICA testing. Moreover, there is direct evidence, provided by 2
prospective and 2 retrospective studies, that compares health outcomes observed during 90-day
to 1-year follow-up for strategies using CCTA particularly in combination with selective FFR-CT
with strategies using ICA or other noninvasive imaging tests. The available evidence provides
support that use of CCTA with selective FFR-CT is likely to reduce the use of ICA in individuals
with stable chest pain who are unlikely to benefit from revascularization by demonstrating the
absence of functionally significant obstructive CAD. In addition, the benefits are likely to
outweigh potential harms because rates of revascularization for functionally significant
obstructive CAD appear to be similar and treatment-related adverse events do not appear to
increase following CCTA with a selective FFR-CT strategy. While individual studies are noted to
have specific methodologic limitations and some variation has been noted in the magnitude of
benefit across studies, in aggregate the evidence provides reasonable support that the selective
addition of FFR-CT following CCTA results in a meaningful improvement in the net health
outcome. The evidence is sufficient to determine that the technology results in meaningful
improvements in the net health outcome.
Practice Guidelines and Position Statements
National Institute for Health and Care Excellence
In 2017, the National Institute for Health and Care Excellence endorsed fractional flow reserve
using coronary computed tomography angiography (FFR-CT), with the following conclusions:
“The committee concluded that the evidence suggests that HeartFlow FFRCT is safe, has high

Blue Cross Idaho
diagnostic accuracy, and that its use may avoid the need for invasive investigations.”55
Recommendations included:
• “The case for adopting HeartFlow FFR-CT for estimating fractional flow reserve from coronary
CT angiography (CCTA) is supported by the evidence. The technology is non-invasive and safe,
and has a high level of diagnostic accuracy.”
• “HeartFlow FFR-CT should be considered as an option for patients with stable, recent onset
chest pain who are offered CCTA as part of the NICE pathway on chest pain. Using HeartFlow
FFR-CT may avoid the need for invasive coronary angiography and revascularization. For
correct use, HeartFlow FFR-CT requires access to 64-slice (or above) CCTA facilities.”
U.S. Preventive Services Task Force Recommendations
Not applicable.
Medicare National Coverage
There is no national coverage determination (NCD). In the absence of an NCD, coverage
decisions are left to the discretion of local Medicare carriers.
Ongoing and Unpublished Clinical Trials
Some currently unpublished trials that might influence this review are listed in Table 6.
Table 6. Summary of Key Trials
Planned
Completion
NCT No.
Trial Name
Enrollment Date
Ongoing
Computed TomogRaphic
Evaluation of Atherosclerotic
NCT02173275
618
Jul 2017
DEtermiNants of Myocardial
IsChEmia
Diagnostic Imaging Strategies
for Patients With Stable Chest
Pain and Intermediate Risk of
Coronary Artery Disease:
NCT02400229
Comparative Effectiveness
3546
Sept 2019
Research of Existing
Technologies) - A Pragmatic
Randomised Controlled Trial of
CT Versus ICA
Assessment of Fractional Flow
reservE Computed
Tomography Versus Single
Photon Emission Computed
NCT02973126
270
Oct 2020
Tomography in the Diagnosis
of Hemodynamically Significant
Coronary Artery Disease.
(AFFECTS)
Assessing Diagnostic Value of
NCT02499679a Non-invasive FFRCT in
5000
Feb 2021
Coronary Care (ADVANCE)
Prospective Evaluation of
NCT02208388
1000
Apr 2024

Blue Cross Idaho
NCT02208388
1000
Apr 2024
MyocaRdial PerFUSion
Planned Completion
NCT No.
Trial Name
Tomography Trial
Enrollment Date
Unpublished
Coronary Computed
Mar 2016
NCT01810198a Tomographic Angiography for
1631
Selective Cardiac
(completed)
Catheterization (CONSERVE)
Machine leArning Based CT
Jan 2017
NCT02805621 angiograpHy derIved FFR: a
352
(completed)
Multi-ceNtEr, Registry
NCT: national clinical trial. a Denotes industry-sponsored or cosponsored trial.
References:
1.
Patel MR, Peterson ED, Dai D, et al. Low diagnostic yield of elective coronary angiography.
N Engl J Med. Mar 11 2010;362(10):886-895. PMID 20220183
2.
Boden WE, O'Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for
stable coronary disease. N Engl J Med. Apr 12 2007;356(15):1503-1516. PMID 17387127
3.
Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS
Guideline for the diagnosis and management of patients with stable ischemic heart
disease: a report of the American College of Cardiology Foundation/American Heart
Association Task Force on Practice Guidelines, and the American College of Physicians,
American Association for Thoracic Surgery, Preventive Cardiovascular Nurses
Association, Society for Cardiovascular Angiography and Interventions, and Society of
Thoracic Surgeons. J Am Coll Cardiol. Dec 18 2012;60(24):e44-e164. PMID 23182125
4.
Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of
coronary-artery disease. N Engl J Med. Jun 14 1979;300(24):1350-1358. PMID 440357
5.
Genders TS, Steyerberg EW, Alkadhi H, et al. A clinical prediction rule for the diagnosis of
coronary artery disease: validation, updating, and extension. Eur Heart J. Jun
2011;32(11):1316-1330. PMID 21367834
6.
Wasfy MM, Brady TJ, Abbara S, et al. Comparison of the Diamond-Forrester method and
Duke Clinical Score to predict obstructive coronary artery disease by computed
tomographic angiography. Am J Cardiol. Apr 01 2012;109(7):998-1004. PMID 22236462
7.
Versteylen MO, Joosen IA, Shaw LJ, et al. Comparison of Framingham, PROCAM,
SCORE, and Diamond Forrester to predict coronary atherosclerosis and cardiovascular
events. J Nucl Cardiol. Oct 2011;18(5):904-911. PMID 21769703
8.
Min JK, Dunning A, Gransar H, et al. Medical history for prognostic risk assessment and
diagnosis of stable patients with suspected coronary artery disease. Am J Med. Aug
2015;128(8):871-878. PMID 25865923
9.
Genders TS, Steyerberg EW, Hunink MG, et al. Prediction model to estimate presence of
coronary artery disease: retrospective pooled analysis of existing cohorts. BMJ. Jun 12
2012;344:e3485. PMID 22692650
10.
CAD Consortium. Pre-test probability of CAD. 2016;
Accessed June 1, 2017.
11.
De Bruyne B, Fearon WF, Pijls NH, et al. Fractional flow reserve-guided PCI for stable
coronary artery disease. N Engl J Med. Sep 25 2014;371(13):1208-1217. PMID 25176289
12.
De Bruyne B, Pijls NH, Kalesan B, et al. Fractional flow reserve-guided PCI versus medical
therapy in stable coronary disease. N Engl J Med. Sep 13 2012;367(11):991-1001. PMID
22924638
13.
Tonino PA, De Bruyne B, Pijls NH, et al. Fractional flow reserve versus angiography for

Blue Cross Idaho
guiding percutaneous coronary intervention. N Engl J Med. Jan 15 2009;360(3):213-224.
PMID 19144937
14.
Pothineni NV, Shah NS, Rochlani Y, et al. U.S. trends in inpatient utilization of fractional
flow reserve and percutaneous coronary intervention. J Am Coll Cardiol. Feb 16
2016;67(6):732-733. PMID 26868697
15.
Blue Cross Blue Shield Association Technology Evaluation Center (TEC). Fractional Flow
Reserve and Coronary Artery Revascularization. TEC Assessment. June 2011;26:Tab 2.
16.
Fearon WF, Shilane D, Pijls NH, et al. Cost-effectiveness of percutaneous coronary
intervention in patients with stable coronary artery disease and abnormal fractional flow
reserve. Circulation. Sep 17 2013;128(12):1335-1340. PMID 23946263
17.
van Nunen LX, Zimmermann FM, Tonino PA, et al. Fractional flow reserve versus
angiography for guidance of PCI in patients with multivessel coronary artery disease
(FAME): 5-year follow-up of a randomised controlled trial. Lancet. Nov 7
2015;386(10006):1853-1860. PMID 26333474
18.
Montalescot G, Sechtem U, Achenbach S, et al. 2013 ESC guidelines on the management
of stable coronary artery disease: the Task Force on the management of stable coronary
artery disease of the European Society of Cardiology. Eur Heart J. Oct 2013;34(38):2949-
3003. PMID 23996286
19.
Windecker S, Kolh P, Alfonso F, et al. 2014 ESC/EACTS Guidelines on myocardial
revascularization: The Task Force on Myocardial Revascularization of the European
Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery
(EACTS) Developed with the special contribution of the European Association of
Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. Oct 1 2014;35(37):2541-
2619. PMID 25173339
20.
Patel MR, Calhoon JH, Dehmer GJ, et al. ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS
2017 Appropriate Use Criteria for coronary revascularization in patients with stable
ischemic heart disease: a report of the American College of Cardiology Appropriate Use
Criteria Task Force, American Association for Thoracic Surgery, American Heart
Association, American Society of Echocardiography, American Society of Nuclear
Cardiology, Society for Cardiovascular Angiography and Interventions, Society of
Cardiovascular Computed Tomography, and Society of Thoracic Surgeons. J Am Coll
Cardiol. May 02 2017;69(17):2212-2241. PMID 28291663
21.
Pijls NH, Van Gelder B, Van der Voort P, et al. Fractional flow reserve. A useful index to
evaluate the influence of an epicardial coronary stenosis on myocardial blood flow.
Circulation. Dec 1 1995;92(11):3183-3193. PMID 7586302
22.
de Bruyne B, Bartunek J, Sys SU, et al. Simultaneous coronary pressure and flow velocity
measurements in humans. Feasibility, reproducibility, and hemodynamic dependence of
coronary flow velocity reserve, hyperemic flow versus pressure slope index, and fractional
flow reserve. Circulation. Oct 15 1996;94(8):1842-1849. PMID 8873658
23.
HeartFlow. DEN130045, FFRct V. 1.4. 2013;
http://www.accessdata.fda.gov/cdrh_docs/reviews/DEN130045.pdf. Accessed September
11, 2016.
24.
Koo BK, Erglis A, Doh JH, et al. Diagnosis of ischemia-causing coronary stenoses by
noninvasive fractional flow reserve computed from coronary computed tomographic
angiograms. Results from the prospective multicenter DISCOVER-FLOW (Diagnosis of
Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) study. J
Am Coll Cardiol. Nov 1 2011;58(19):1989-1997. PMID 22032711
25.
Min JK, Koo BK, Erglis A, et al. Effect of image quality on diagnostic accuracy of
noninvasive fractional flow reserve: results from the prospective multicenter international
DISCOVER-FLOW study. J Cardiovasc Comput Tomogr. May-Jun 2012;6(3):191-199.
PMID 22682261
26.
Nakazato R, Park HB, Berman DS, et al. Noninvasive fractional flow reserve derived from
computed tomography angiography for coronary lesions of intermediate stenosis severity:
results from the DeFACTO study. Circ Cardiovasc Imaging. Nov 2013;6(6):881-889. PMID
24081777

Blue Cross Idaho
27.
Nørgaard BL, Leipsic J, Gaur S, et al. Diagnostic performance of noninvasive fractional
flow reserve derived from coronary computed tomography angiography in suspected
coronary artery disease: the NXT trial (Analysis of Coronary Blood Flow Using CT
Angiography: Next Steps). J Am Coll Cardiol. Apr 1 2014;63(12):1145-1155. PMID
24486266
28.
Taylor CA, Fonte TA, Min JK. Computational fluid dynamics applied to cardiac computed
tomography for noninvasive quantification of fractional flow reserve: scientific basis. J Am
Coll Cardiol. Jun 4 2013;61(22):2233-2241. PMID 23562923
29.
Kim KH, Doh JH, Koo BK, et al. A novel noninvasive technology for treatment planning
using virtual coronary stenting and computed tomography-derived computed fractional flow
reserve. JACC Cardiovasc Interv. Jan 2014;7(1):72-78. PMID 24332418
30.
HeartFlow. K152733, FFRct v2.0. 2016;
https://www.accessdata.fda.gov/cdrh_docs/pdf15/K152733.pdf. Accessed September 11,
2016.
31.
Johnson NP, Johnson DT, Kirkeeide RL, et al. Repeatability of fractional flow reserve
despite variations in systemic and coronary hemodynamics. JACC Cardiovasc Interv. Jul
2015;8(8):1018-1027. PMID 26205441
32.
Hulten E, Di Carli MF. FFRCT: Solid PLATFORM or thin iceZ J Am Coll Cardiol. Dec 1
2015;66(21):2324-2328. PMID 26475206
33.
Gaur S, Bezerra HG, Lassen JF, et al. Fractional flow reserve derived from coronary CT
angiography: variation of repeated analyses. J Cardiovasc Comput Tomogr. Jul-Aug
2014;8(4):307-314. PMID 25151923
34.
Nørgaard BL, Gaur S, Leipsic J, et al. Influence of coronary calcification on the diagnostic
performance of CT angiography derived FFR in coronary artery disease: a substudy of the
NXT Trial. JACC Cardiovasc Imaging. Sep 2015;8(9):1045-1055. PMID 26298072
35.
Takx RA, Blomberg BA, El Aidi H, et al. Diagnostic accuracy of stress myocardial perfusion
imaging compared to invasive coronary angiography with fractional flow reserve meta-
analysis. Circ Cardiovasc Imaging. Jan 2015;8(1). PMID 25596143
36.
Wu W, Pan DR, Foin N, et al. Noninvasive fractional flow reserve derived from coronary
computed tomography angiography for identification of ischemic lesions: a systematic
review and meta-analysis. Sci Rep. 2016;6:29409. PMID 27377422
37.
Danad I, Szymonifka J, Twisk JWR, et al. Diagnostic performance of cardiac imaging
methods to diagnose ischaemia-causing coronary artery disease when directly compared
with fractional flow reserve as a reference standard: a meta-analysis. Eur Heart J. Apr 01
2017;38(13):991-998. PMID 27141095
38.
Renker M, Schoepf UJ, Wang R, et al. Comparison of diagnostic value of a novel
noninvasive coronary computed tomography angiography method versus standard
coronary angiography for assessing fractional flow reserve. Am J Cardiol. Nov 01
2014;114(9):1303-1308. PMID 25205628
39.
De Geer J, Sandstedt M, Bjorkholm A, et al. Software-based on-site estimation of fractional
flow reserve using standard coronary CT angiography data. Acta Radiol. Oct
2016;57(10):1186-1192. PMID 26691914
40.
Min JK, Leipsic J, Pencina MJ, et al. Diagnostic accuracy of fractional flow reserve from
anatomic CT angiography. JAMA. Sep 26 2012;308(12):1237-1245. PMID 22922562
41.
Thompson AG, Raju R, Blanke P, et al. Diagnostic accuracy and discrimination of ischemia
by fractional flow reserve CT using a clinical use rule: results from the Determination of
Fractional Flow Reserve by Anatomic Computed Tomographic Angiography study. J
Cardiovasc Comput Tomogr. Mar-Apr 2015;9(2):120-128. PMID 25819194
42.
Whiting PF, Rutjes AW, Westwood ME, et al. QUADAS-2: a revised tool for the quality
assessment of diagnostic accuracy studies. Ann Intern Med. Oct 18 2011;155(8):529-536.
PMID 22007046
43.
Coenen A, Lubbers MM, Kurata A, et al. Fractional flow reserve computed from
noninvasive CT angiography data: diagnostic performance of an on-site clinician-operated
computational fluid dynamics algorithm. Radiology. Mar 2015;274(3):674-683. PMID
25322342

Blue Cross Idaho
44.
PROSPERO. International prospective register of systematic reviews. n.d.;
https://www.crd.york.ac.uk/PROSPERO/. Accessed April 28, 2017.
45.
Min JK, Berman DS, Budoff MJ, et al. Rationale and design of the DeFACTO
(Determination of Fractional Flow Reserve by Anatomic Computed Tomographic
AngiOgraphy) study. J Cardiovasc Comput Tomogr. Sep-Oct 2011;5(5):301-309. PMID
21930103
46.
Curzen NP, Nolan J, Zaman AG, et al. Does the routine availability of CT-derived FFR
Influence management of patients with stable chest pain compared to CT angiography
aloneZ: The FFRCT RIPCORD Study. JACC Cardiovasc Imaging. Oct 2016;9(10):1188-
1194. PMID 27568119
47.
Douglas PS, De Bruyne B, Pontone G, et al. 1-year outcomes of FFRCT-guided care in
patients with suspected coronary disease: the PLATFORM Study. J Am Coll Cardiol. Aug 2
2016;68(5):435-445. PMID 27470449
48.
Douglas PS, Pontone G, Hlatky MA, et al. Clinical outcomes of fractional flow reserve by
computed tomographic angiography-guided diagnostic strategies vs. usual care in patients
with suspected coronary artery disease: the prospective longitudinal trial of FFR(CT):
outcome and resource impacts study. Eur Heart J. Dec 14 2015;36(47):3359-3367. PMID
26330417
49.
Hlatky MA, De Bruyne B, Pontone G, et al. Quality-of-life and economic outcomes of
assessing fractional flow reserve with computed tomography angiography: PLATFORM. J
Am Coll Cardiol. Dec 1 2015;66(21):2315-2323. PMID 26475205
50.
Dewey M, Rief M, Martus P, et al. Evaluation of computed tomography in patients with
atypical angina or chest pain clinically referred for invasive coronary angiography:
randomised controlled trial. Bmj. Oct 24 2016;355:i5441. PMID 27777234
51.
Moller Jensen J, Erik Botker H, Norling Mathiassen O, et al. Computed tomography
derived fractional flow reserve testing in stable patients with typical angina pectoris:
influence on downstream rate of invasive coronary angiography. Eur Heart J Cardiovasc
Imaging. Apr 20 2017. PMID 28444153
52.
Nørgaard BL, Hjort J, Gaur S, et al. Clinical use of coronary CTA-derived FFR for decision-
making in stable CAD. JACC Cardiovasc Imaging. May 2017;10(5):541-550. PMID
27085447
53.
Lu MT, Ferencik M, Roberts RS, et al. Noninvasive FFR Derived From Coronary CT
Angiography: Management and Outcomes in the PROMISE Trial. JACC Cardiovasc
Imaging. Apr 07 2017. PMID 28412436
54.
Douglas PS, Hoffmann U, Lee KL, et al. PROspective Multicenter Imaging Study for
Evaluation of chest pain: rationale and design of the PROMISE trial. Am Heart J. Jun
2014;167(6):796-803 e791. PMID 24890527
55.
National Institute for Health and Care Excellence. HeartFlow FFRCT for estimating
fractional flow reserve from coronary CT angiography [MTG32]. 2017;
https://www.nice.org.uk/guidance/mtg32. Accessed April 28, 2017.
CODES
Codes Number Description
No specific code for fractional flow
CPT
reserve
Computed tomographic angiography, heart,
coronary arteries and bypass grafts (when
present), with contrast material, including 3D
75574
image postprocessing (including evaluation of
cardiac structure and morphology, assessment of
cardiac function, and evaluation of venous
structures, if performed).
HCPCS
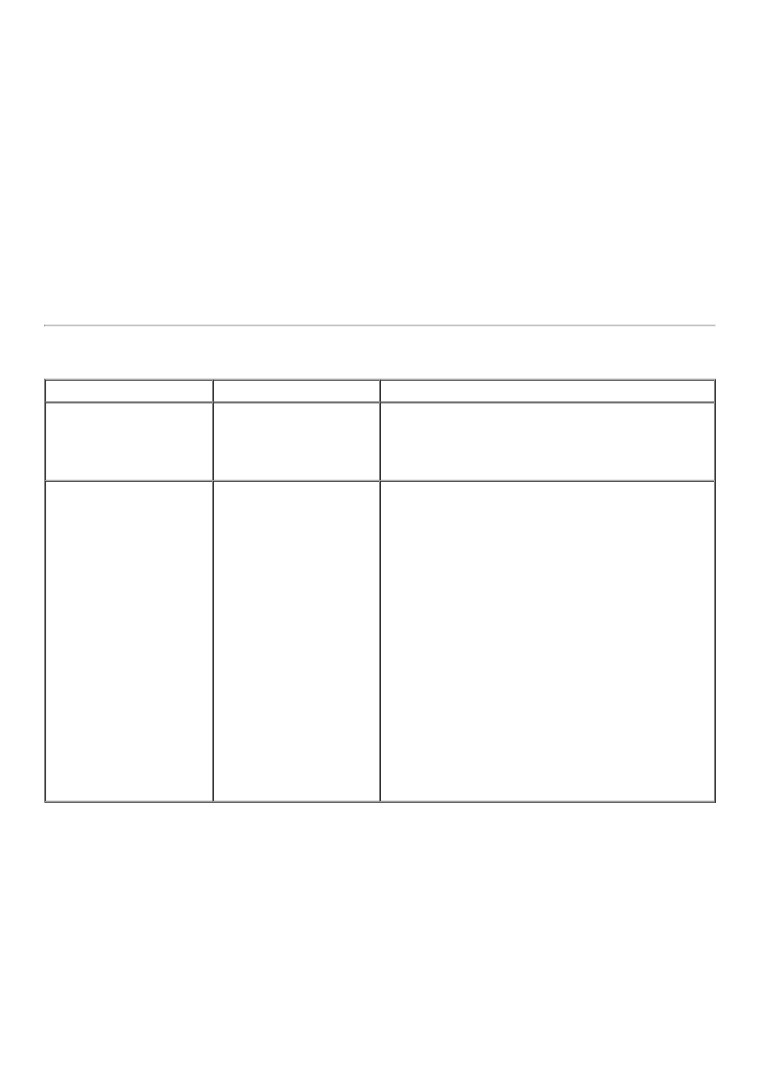
Blue Cross Idaho
ICD-10-
Angina pectoris, unspecified (includes ischemic
I20.9
CM
chest pain)
Atherosclerotic heart disease of native coronary
I25.118-
artery with angina pectoris other than unstable or
I25.119
with documented spasm
ICD-10-PCS codes are only used for inpatient
ICD-10-
services. There is no specific ICD-10-PCS code
PCS
for this procedure.
Type of
service
Place of
service
Policy History
Date
Action
Reason
Policy created with literature review through
New Policy - Add to
October 27, 2016. Use of FFR-CT in patients
1/18/17
Radiology section
with suspected stable ischemic heart disease is
considered investigational.
Policy renamed and updated with literature
review through April 11, 2017, and a new
literature submission from HeartFlow; several
new references added. Clinical context and
formulation extensively revised. Policy
statement updated to medically necessary for
individuals with stable chest pain at
intermediate risk of coronary artery disease
7/25/17
Replace policy
being considered for invasive coronary
angiography; “positive” added before CCTA to
more explicitly state that FFR-CT is intended
for selective use following CCTA with positive
results. Background and Policy Guideline
sections revised with addition of information
about clinical prediction scores and patient
selection criteria related to technical image
quality.